If you’ve had a stubborn, itchy rash that keeps coming back no matter what creams you use, you’re not alone. About contact dermatitis affects millions of people every year - and for many, the real problem isn’t dry skin or bad hygiene. It’s something you’re touching every day without realizing it.
What Exactly Is Contact Dermatitis?
Contact dermatitis isn’t one thing. It’s your skin’s delayed reaction to something it’s touched. Think of it like a slow-burning fuse. You touch something - maybe your watch, your shampoo, or your work gloves - and 24 to 72 hours later, your skin starts to burn, blister, or peel. It’s not contagious. It’s not an infection. It’s an allergic response, and it’s surprisingly common.
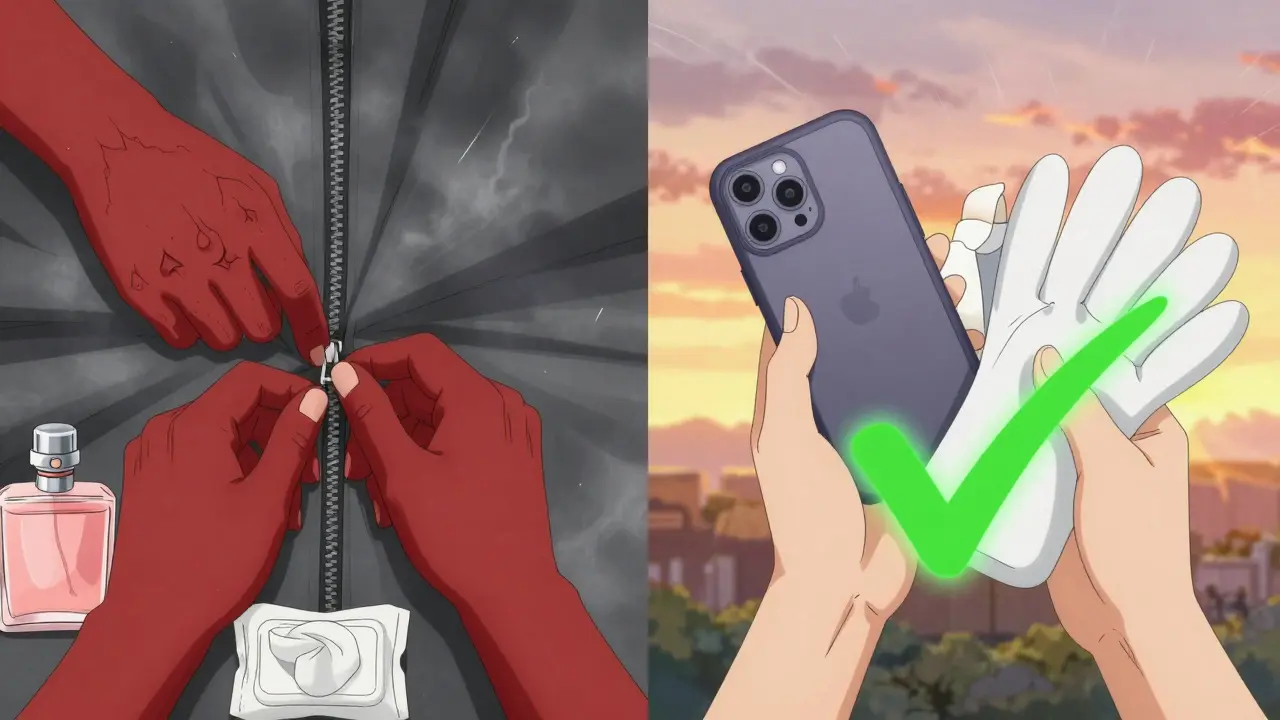
Up to 20% of all contact dermatitis cases are allergic in nature, according to dermatology research. That means your immune system has learned to see a harmless chemical as a threat. Once it does, every future touch triggers inflammation. The most common culprit? Nickel. It’s in jewelry, belt buckles, zippers, even some smartphones. In North America, nearly 1 in 6 women and 1 in 30 men test positive for nickel allergy. And it’s not just metals. Fragrances, preservatives, and even natural plant extracts can set off reactions.
How Do You Know What’s Causing It?
Guessing won’t cut it. You can’t just stop using everything that touches your skin. That’s where patch testing comes in - the gold standard for finding the exact trigger.
Unlike skin prick tests for pollen or food allergies, patch testing looks for delayed reactions. It’s simple: small amounts of 29 common allergens are taped to your back in tiny patches. You leave them on for 48 hours, then return for the first reading. You come back again at 96 hours for the final check. The whole process takes about four days.
The standard test - called the TRUE Test - includes things like nickel sulfate, cobalt chloride, fragrance mix, and balsam of Peru. These are the usual suspects. But here’s the catch: there are thousands of possible allergens out there. The standard panel only covers the most common ones. If your rash keeps coming back despite a negative result, you might need expanded testing. Some clinics now test for 70 to 100 allergens, especially if you work in healthcare, hairdressing, or construction.
One patient on Reddit said after five years of rashes, patch testing finally revealed she was allergic to cocamidopropyl betaine - a foaming agent in shampoos and body washes. Once she switched brands, her hands cleared up completely. Another person had a false negative on nickel. It took a second, more detailed test to find formaldehyde in her makeup.
What Are the Most Common Allergens?
Here’s what actually shows up in patch tests, based on real clinical data:
- Nickel sulfate - 14.7% of positive cases. Found in jewelry, coins, keys, phone cases, and even some eyeglass frames.
- Cobalt chloride - 4.8%. Often paired with nickel in metal alloys. Also in some paints and cement.
- Fragrance mix - 3.4%. A blend of 8 common scents used in perfumes, lotions, and detergents.
- Balsam of Peru - 3.0%. Used in cosmetics, foods (like cinnamon and citrus), and even some toothpastes.
- Thimerosal - 5.0%. A preservative in some eye drops and vaccines (rarely in cosmetics anymore).
- Formaldehyde - found in nail polish, shampoos, and some disinfectants.
- Chromates - in cement, leather, and some paints. A big issue for construction workers.
And don’t forget: “fragrance-free” doesn’t always mean safe. Many products replace traditional fragrances with botanical extracts like tea tree oil, lavender, or eucalyptus - all of which can trigger reactions too. If you’re allergic to fragrance mix, you might still react to these natural alternatives.
How Do You Avoid These Triggers?
Knowing your allergen is only half the battle. Avoiding it is the other half - and it’s harder than you think.
Here’s how to start:
- Read labels. Look for the exact name of your allergen. Nickel? Avoid anything labeled “nickel-plated” or “metal alloy.” Fragrance? Look for “parfum,” “fragrance,” or “essential oil.”
- Use the Contact Allergen Replacement Database (CARD). Run by the American Contact Dermatitis Society, CARD lists safe alternatives for 27 common allergens. For example, if you’re allergic to formaldehyde, it will suggest shampoos and lotions that don’t contain it.
- Test new products. Before using a new lotion or detergent, put a small amount on your inner forearm. Wait 48 hours. If no reaction, it’s probably safe.
- Switch to hypoallergenic tools. If you’re allergic to nickel, use plastic or titanium zippers. Replace metal buttons with fabric ones. Use a silicone phone case instead of metal.
- Protect your skin at work. If you’re a hairdresser, nurse, or mechanic, wear gloves - but make sure they’re not made of latex or contain rubber accelerators. Cotton-lined gloves are often safer.
One study found that 82% of people saw big improvements after avoiding their identified allergens. But 47% struggled to find hidden sources. That’s because allergens hide in plain sight: in your laundry detergent, your baby’s wipes, your yoga mat, your kitchen sponge.
What About Occupational Exposure?
Work is where most serious cases happen. About 90% of contact dermatitis in industrial jobs is allergic. Hairdressers? 42% have reactions - usually to paraphenylenediamine in hair dye. Healthcare workers? 26% react to latex or disinfectants. Construction workers? Chromates in cement cause hand eczema.
Employers in the EU are required to reduce exposure under REACH regulations. In the U.S., OSHA doesn’t have the same rules. That means if you’re in a high-risk job, you might need to push for safer materials. Talk to your occupational health team. Bring your patch test results. Ask for alternatives.
What’s New in Diagnosis and Treatment?
The field is changing. In 2025, the American Contact Dermatitis Society is expanding its standard patch test from 29 to 80 allergens. That includes newer triggers like chemicals in smartwatches, green cosmetics, and plant-based cleansers.
Scientists are also looking at blood markers. One study found that IL-18 levels in the blood rise with ACD severity. That could one day mean a simple blood test replaces the patch test - but not yet. Right now, nothing beats the patch test for accuracy.
And animal testing? It’s being phased out. The EU banned guinea pig tests in 2013 and will fully eliminate them by 2027. New methods use human skin cells in labs - faster, more ethical, and just as reliable.
What If the Test Comes Back Negative?
If you still have a rash after patch testing, it might not be allergic contact dermatitis. It could be irritant contact dermatitis - caused by repeated exposure to soaps, solvents, or water. Or it could be eczema, psoriasis, or even a fungal infection.
Don’t give up. Go back to your dermatologist. Ask for a biopsy. Ask about other triggers. Sometimes, the answer isn’t in the patch test - it’s in your daily habits.
Can You Outgrow a Contact Allergy?
Usually, no. Once your immune system reacts to an allergen, it remembers. But you can reduce your exposure enough to stay symptom-free. And in some cases, strict avoidance for years can lead to reduced sensitivity.
That’s why nickel allergy rates dropped by 25% in the EU after laws restricted nickel in jewelry and buttons. The same could happen here - if consumers demand safer products.
What Should You Do Next?
If you’ve had a recurring rash for more than a few weeks:
- Stop guessing. See a dermatologist who does patch testing.
- Bring a list of everything you put on your skin - soaps, lotions, makeup, laundry detergent.
- Ask if expanded testing is needed.
- Get your results in writing. Save them.
- Use CARD or similar databases to find safe products.
- Don’t trust labels like “natural” or “hypoallergenic” - they’re not regulated.
It’s not about living in fear. It’s about knowing what to avoid - and what’s safe. Once you find the trigger, your skin can heal. And you won’t have to live with the itch anymore.
Can contact dermatitis be cured?
There’s no permanent cure for allergic contact dermatitis because once your immune system reacts to an allergen, it usually remembers it. But you can completely control it by avoiding the trigger. Most people see major improvement - or total clearance - once they stop contact with the allergen. It’s not about healing the skin; it’s about stopping the exposure.
How long does patch testing take?
Patch testing typically takes four days. Patches are applied on Monday, read on Wednesday (after 48 hours), and read again on Friday (after 96 hours). You must keep the area dry and avoid sweating or removing the patches during that time. Results are most accurate when read at 96 hours, as some reactions take longer to appear.
Is patch testing painful?
No, patch testing isn’t painful. The patches are taped to your back and don’t involve needles or pricks. You might feel mild itching or burning if you’re allergic to one of the substances - but that’s the point. The test is designed to cause a reaction, not pain. Some people find the tape uncomfortable or itchy, but it’s generally well-tolerated.
Can I do patch testing at home?
No, patch testing should never be done at home. It requires trained professionals to apply the patches correctly, interpret the results accurately, and manage any strong reactions. DIY tests or online kits are unreliable and can cause severe irritation or false results. Always see a board-certified dermatologist or allergist.
What if my patch test is negative but I still have a rash?
A negative patch test doesn’t rule out contact dermatitis. You might have irritant contact dermatitis, which isn’t allergic but caused by repeated exposure to harsh chemicals. Or it could be another skin condition like eczema or psoriasis. Your doctor may recommend a skin biopsy, blood tests, or a trial elimination of common irritants. Don’t assume the test was wrong - ask for next steps.
Are natural products safer for sensitive skin?
Not necessarily. Many natural ingredients - like tea tree oil, lavender, citrus extracts, and even essential oils - are common allergens. Products labeled “natural” or “organic” often contain plant-based fragrances that trigger reactions. Always check the ingredient list, even for natural brands. If you’re allergic to fragrance mix, avoid anything with “essential oil” or “fragrance” - no matter how it’s marketed.
How long does it take for a rash to improve after avoiding the allergen?
Most people see improvement within 2 to 4 weeks after removing the allergen. Some see changes in just a few days. If there’s no improvement after a month, the allergen might not be the only trigger - or you might still be exposed unknowingly. Check your environment: laundry detergents, towels, workplace surfaces, and even pets can carry allergens.
Can children get allergic contact dermatitis?
Yes, children can develop allergic contact dermatitis, though it’s less common than in adults. Nickel is a top trigger in kids - often from belt buckles, jeans buttons, or jewelry. Diapers, wet wipes, and baby lotions can also contain allergens. If a child has persistent diaper rash or eczema that doesn’t respond to creams, patch testing may be recommended, especially if there’s a family history of allergies.


Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.