Renal Dosing Calculator for Elderly Patients
Patient Information
Medication Selection
Estimated Creatinine Clearance (CrCl)
Recommended Dose
Safety Warning
When kidneys start to slow down in older adults, even normal doses of common medications can become dangerous. It’s not just about age-it’s about how the body handles drugs when kidney function drops. Around 38% of people over 65 have chronic kidney disease, and many of them are taking medications that can build up to toxic levels if not adjusted properly. This isn’t a rare issue. It’s happening in homes, nursing facilities, and hospitals every day, often unnoticed until someone falls, gets confused, or ends up back in the ER.
Why Kidney Function Matters for Medications
Your kidneys don’t just make urine. They filter your blood, removing waste and excess drugs. When kidney function declines, those drugs stick around longer. For some medications, that means they build up to dangerous levels. This is especially risky for older adults because their bodies don’t handle drugs the same way they did at 30. Muscle mass drops, body water changes, and liver function slows down-all of it affects how drugs move through the system. The key number doctors look at is glomerular filtration rate (GFR). A GFR below 60 mL/min/1.73 m² means kidney function is impaired. But here’s the catch: many doctors still rely on serum creatinine alone, which can be misleading in older people. Creatinine comes from muscle, and older adults often have less muscle. So even if their creatinine looks normal, their kidneys might be working at only 40% capacity.How to Measure Kidney Function Accurately
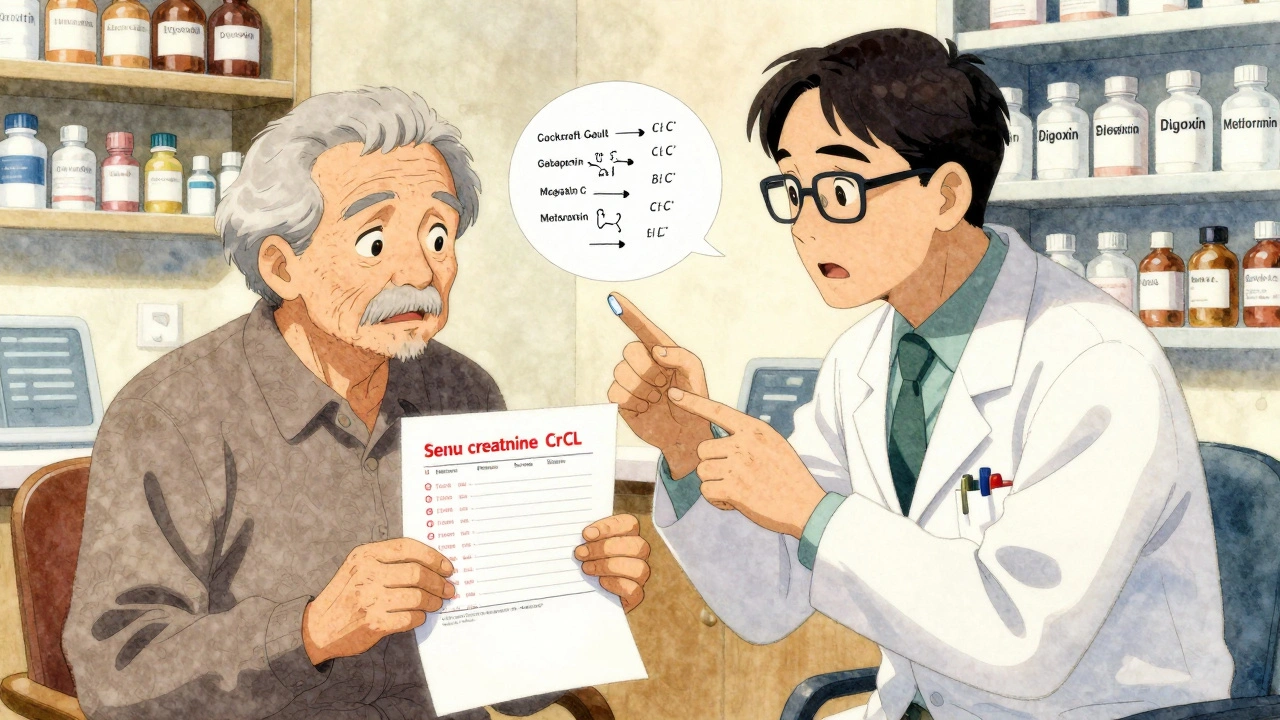
The most common way to estimate kidney function is with the Cockcroft-Gault equation. It uses age, weight, sex, and serum creatinine to calculate creatinine clearance (CrCl). The formula looks like this:CrCl = [(140 − age) × weight (kg)] ÷ (72 × serum creatinine) × 0.85 (if female)
But this equation has a flaw: it often underestimates kidney function in older adults by 15-20%. That means if the calculation says CrCl is 45 mL/min, the real number might be closer to 55. If you reduce the dose too much based on that, the patient might not get enough medicine.
That’s why guidelines now recommend using cystatin C for more accurate results in elderly patients. Cystatin C isn’t affected by muscle mass, so it gives a clearer picture. For patients with borderline kidney function-say, GFR around 29-31 mL/min-using both creatinine-based and cystatin C-based estimates helps avoid mistakes.
Medications That Need Special Care
Not all drugs are created equal when it comes to kidney clearance. Some are safe. Others? Not even close.- Metformin: This common diabetes drug is cleared almost entirely by the kidneys. In the U.S., guidelines say to stop it if serum creatinine is above 1.5 mg/dL in men or 1.4 mg/dL in women. But in Europe, doctors can keep using it with close monitoring. The risk? Lactic acidosis-a rare but deadly buildup of acid in the blood.
- Gabapentin: Used for nerve pain and seizures, it’s one of the most commonly misdosed drugs in older adults. About 68% of prescribers get it wrong. For CrCl below 30 mL/min, the dose should drop from 300-1200 mg daily to 100-300 mg daily. Too much can cause dizziness, falls, and confusion.
- Allopurinol: For gout, this drug can cause severe skin reactions if not dosed right. In severe kidney impairment (GFR under 10 mL/min), start with 100 mg every other day, not daily. Many still give the standard 100 mg daily, putting patients at risk.
- Digoxin: This heart medication has a very narrow safety window. Therapeutic levels are between 0.8 and 2.0 ng/mL. Too high? Irregular heartbeat, nausea, even death. In elderly patients with kidney issues, levels should be checked 15-20 days after starting, not 5-7 days like in younger people.
- Lithium: Used for bipolar disorder, lithium is cleared almost entirely by the kidneys. Even small drops in kidney function can cause toxicity. The safe range is 0.6-0.8 mmol/L for long-term use. Many older patients on lithium need monthly blood tests.
Some drugs don’t need adjustment at all. Glipizide, another diabetes medicine, is metabolized by the liver and doesn’t rely on kidneys. That makes it safer for elderly patients with kidney disease.
Dosing Strategies That Actually Work
There are three main ways to adjust doses for kidney impairment:- Dose reduction: Lower the amount per dose. For example, gabapentin drops from 600 mg three times a day to 100-300 mg once a day.
- Interval extension: Keep the same dose but give it less often. Vancomycin might go from every 12 hours to every 48 hours.
- Combination approach: Reduce the dose AND extend the interval. Piperacillin/tazobactam might go from 3.375g every 6 hours to 2.25g every 8 hours.
Some prescribers use the “50% rule”-if a drug is 50% or more cleared by the kidneys, cut the dose in half when CrCl drops below 50 mL/min. But that’s risky. About 22% of high-risk drugs don’t follow this rule. Vancomycin, for example, has nonlinear clearance. Cutting the dose in half might not be enough-or too much.
What Happens When You Get It Wrong
The consequences aren’t theoretical. A 2020 study found that 12-15% of all adverse drug events in elderly patients are due to improper kidney-based dosing. That’s one in eight hospitalizations or ER visits linked to a simple dosing mistake.One patient, 82, was on gabapentin for sciatica. His doctor didn’t adjust the dose after his kidney function dropped. He started stumbling, forgetting names, and falling twice in one month. His CrCl was 28 mL/min. His gabapentin dose was 600 mg three times a day. After switching to 100 mg once daily, his balance improved within a week. No more falls. No more confusion.
Another case: an 80-year-old on digoxin for atrial fibrillation. His levels were checked too early-only 5 days after starting. He was given a standard 0.125 mg daily. His actual level was 3.1 ng/mL-well above toxic. He developed nausea, vomiting, and a dangerous heart rhythm. He spent a week in the hospital. His dose should have been 0.0625 mg daily, and levels should have been checked after 15 days.
Tools That Help Clinicians Get It Right
The best defense against dosing errors is a system-not just a person’s memory.- Electronic health record alerts: The University of Nebraska Medical Center added alerts that pop up when a drug is prescribed to a patient with low CrCl. Within a year, inappropriate dosing dropped by 37%.
- Pharmacist-led reviews: Mayo Clinic found that when clinical pharmacists reviewed all kidney-related doses for patients over 65, adverse events dropped by 58%.
- Mobile apps: Apps like Epocrates Renal Dosing are used over 1.2 million times a year. They pull in lab values and suggest instant adjustments for 150+ drugs.
- AI-powered tools: In 2023, the FDA approved DoseOptima, an AI system that integrates real-time GFR data with drug databases. In trials, it made correct dose recommendations 92.4% of the time.
What’s Changing in 2025
The guidelines are evolving. The Kidney Disease: Improving Global Outcomes (KDIGO) group is finalizing its 2023 update, which will recommend cystatin C as the preferred test for elderly patients. That’s a big shift-from relying on creatinine, which can lie, to using a more accurate marker.The American Society of Health-System Pharmacists (ASHP) is also rolling out a national standard for renal dosing by the end of 2023. It will list exact CrCl thresholds for 150 high-risk medications-no more guesswork.
Meanwhile, the FDA now requires all new drugs targeting patients over 65 to include clear renal dosing instructions on their labels. The European Medicines Agency has had this rule since 2017. The U.S. is finally catching up.
What You Can Do
If you’re caring for an older adult on multiple medications:- Ask for a creatinine clearance (CrCl) calculation-not just serum creatinine.
- Ask if any drugs need adjustment for kidney function. Don’t assume the doctor already checked.
- Request a medication review with a pharmacist, especially if they’ve been hospitalized or had a recent fall.
- Keep a list of all medications, including over-the-counter ones like NSAIDs (ibuprofen, naproxen), which can hurt kidneys too.
- Watch for signs of toxicity: confusion, dizziness, nausea, weakness, or irregular heartbeat.
Medications aren’t one-size-fits-all-especially in older adults. What’s safe for a 50-year-old might be dangerous for an 80-year-old with kidney trouble. The fix isn’t complicated: check kidney function, adjust the dose, and double-check the math. Do that, and you can prevent a lot of harm.
How do I know if an elderly person’s kidneys are working poorly?
The best way is to calculate creatinine clearance (CrCl) using the Cockcroft-Gault equation, which uses age, weight, sex, and serum creatinine. A CrCl under 60 mL/min means kidney function is reduced. But because creatinine can be misleading in older adults, doctors should also check cystatin C for a more accurate picture. Symptoms like swelling, fatigue, or confusion can signal problems, but they’re often missed-so lab tests are essential.
Which medications are most dangerous for elderly patients with kidney problems?
Gabapentin, metformin, allopurinol, digoxin, and lithium are among the highest risk. Gabapentin causes dizziness and falls if not reduced. Metformin can lead to lactic acidosis. Allopurinol may trigger severe skin reactions. Digoxin and lithium have narrow safety windows-small changes in kidney function can push levels into the toxic range. Always check if a drug is primarily cleared by the kidneys.
Can I just cut the dose in half for all medications if kidney function is low?
No. The "50% rule" works for some drugs but fails for others, especially those with nonlinear pharmacokinetics like vancomycin or drugs with active metabolites. Some medications need interval extension instead of dose reduction. Others, like glipizide, don’t need any adjustment at all. Always check specific guidelines for each drug-don’t guess.
Are over-the-counter painkillers safe for older adults with kidney issues?
No. NSAIDs like ibuprofen and naproxen can reduce blood flow to the kidneys and cause acute kidney injury, especially in older adults. Acetaminophen (Tylenol) is safer for kidney function, but it has its own risks at high doses. Always talk to a doctor or pharmacist before using any OTC painkiller regularly.
Should elderly patients stop taking all kidney-cleared medications?
No. Many medications are still safe and necessary-they just need the right dose. Stopping them can be just as dangerous as giving too much. For example, stopping digoxin might cause heart failure to worsen. The goal isn’t to avoid these drugs-it’s to adjust them correctly. Work with a pharmacist to find the safest dose for each medication.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.