Ever taken a pill and felt like it did nothing? You’re not imagining it. For many people, especially those with gut conditions, the problem isn’t the drug-it’s whether the drug even gets into the bloodstream. Gastrointestinal medications face a brutal gauntlet just to work. From stomach acid to intestinal mucus, from slow digestion to inflamed tissue, the body’s own systems can block or delay absorption so badly that a perfectly good drug becomes useless.
Why Your Pill Might Not Be Working
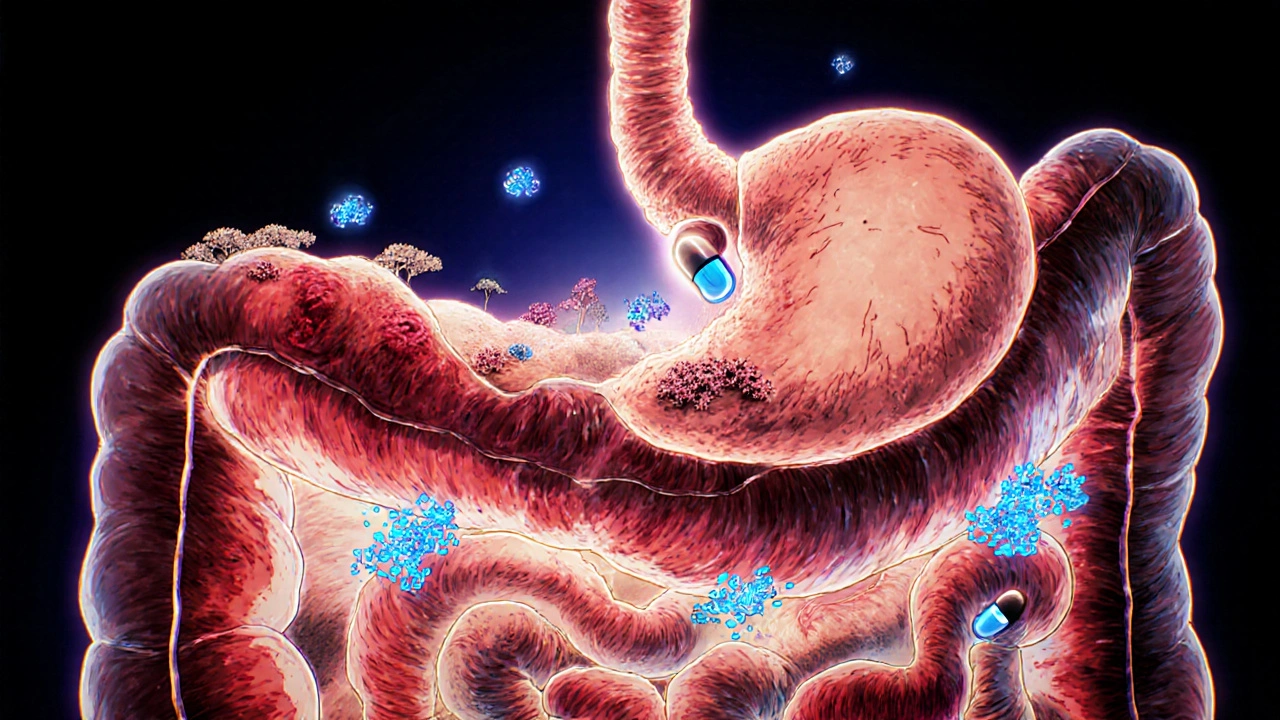
Most pills you swallow are meant to be absorbed in the small intestine. That’s where the magic happens: a surface area bigger than a tennis court, lined with tiny finger-like projections called villi. But getting a drug across that wall isn’t easy. The gut doesn’t just passively let things through. It’s got layers of defense. First, there’s the mucus layer-up to half a millimeter thick in places. It’s like trying to swim through jelly. Then there are enzymes that chew up drugs before they can be absorbed. P-glycoprotein, a molecular pump on intestinal cells, actively kicks out certain drugs back into the gut. And tight junctions between cells? They’re like sealed doors. Only small, fat-soluble molecules slip through easily. If your drug is water-soluble, heavy (over 500 Daltons), or a target for these pumps, your chances of absorption drop hard. Insulin, for example, has a molecular weight of nearly 6,000 Da. Oral insulin? Almost zero absorption. That’s why it’s injected.Food, pH, and Timing: The Silent Saboteurs
You’ve heard to take some meds on an empty stomach. There’s a reason. Food, especially fatty meals, slows gastric emptying by 2 to 4 hours. That means your pill sits in your stomach longer. For drugs like levothyroxine, that delay can cut absorption by 30-50%. The result? Inadequate thyroid hormone levels, fatigue, weight gain-even if you’re taking the right dose. The gut isn’t one uniform tube. It’s a pH gradient. Your stomach is acidic (pH 1.5-3.5). The duodenum jumps to pH 5-6. By the time you reach the lower small intestine, it’s nearly neutral to slightly alkaline (pH 7-8). Drugs change form depending on pH. Acidic drugs like aspirin dissolve better in the stomach. Basic drugs like amoxicillin need the higher pH of the small intestine. If your transit time is off-say, from diarrhea or constipation-the drug might not spend enough time in the right zone to be absorbed.Disease Changes Everything
A healthy gut and an inflamed gut are two different worlds. In Crohn’s disease or ulcerative colitis, the lining is damaged. Villi get flattened. Mucus thickens. Blood flow drops. All of this cuts absorption. Take mesalamine, a common drug for IBD. In healthy people, it’s absorbed about 70% of the time. In someone with active ulcerative colitis? That drops to 30-45%. One patient on a Crohn’s forum said their Remicade levels kept swinging from undetectable to therapeutic-even with perfect dosing. That’s not noncompliance. That’s their gut refusing to let the drug in. Short bowel syndrome is even worse. If you’ve lost half your small intestine, there’s simply not enough surface area to absorb anything. Patients often need 2-3 times the standard dose of antibiotics, vitamins, or even blood thinners just to get the same effect. Nurses report INR levels in warfarin patients with IBD swinging from 1.5 to 4.5 without any dose change. That’s a recipe for clotting or bleeding.
Drug Interactions You Can’t Ignore
Newer medications like semaglutide (Ozempic, Wegovy) slow down gut motility. That sounds good for weight loss-but bad for other drugs. If you’re taking a blood thinner, an antibiotic, or a seizure med, that delay can push your plasma levels too low or too high. For drugs with a narrow therapeutic window-like warfarin, digoxin, or phenytoin-that’s dangerous. Even common OTC drugs interfere. Antacids raise stomach pH, which can stop absorption of drugs that need acid to dissolve. Proton pump inhibitors (PPIs) like omeprazole reduce absorption of vitamin B12, iron, and certain antifungals. And don’t forget fiber. Psyllium or bran can trap drugs in the gut like a sponge, preventing them from reaching the bloodstream.Formulation Matters More Than You Think
A pill isn’t just a pill. It’s a carefully engineered package. The same active ingredient can behave wildly differently depending on whether it’s a regular tablet, a delayed-release capsule, a liquid suspension, or a nanoparticle. Take griseofulvin, an old antifungal. It dissolves so slowly that if your gut moves too fast, you just poop out the drug. Manufacturers solved this by making it into a microcrystalline form-faster dissolution, better absorption. That’s why generic versions sometimes don’t work as well: they use different salt forms or crystal structures. Nanocarriers are the future. Liposomes, solid lipid nanoparticles-these tiny fat bubbles can carry drugs past the mucus, avoid the pumps, and slip right into cells. In trials, they’ve boosted bioavailability by 1.5 to 3.5 times for drugs like paclitaxel or curcumin. But these aren’t widely available yet. Only 15-20% of oral drugs have labeling that even mentions use in IBD patients.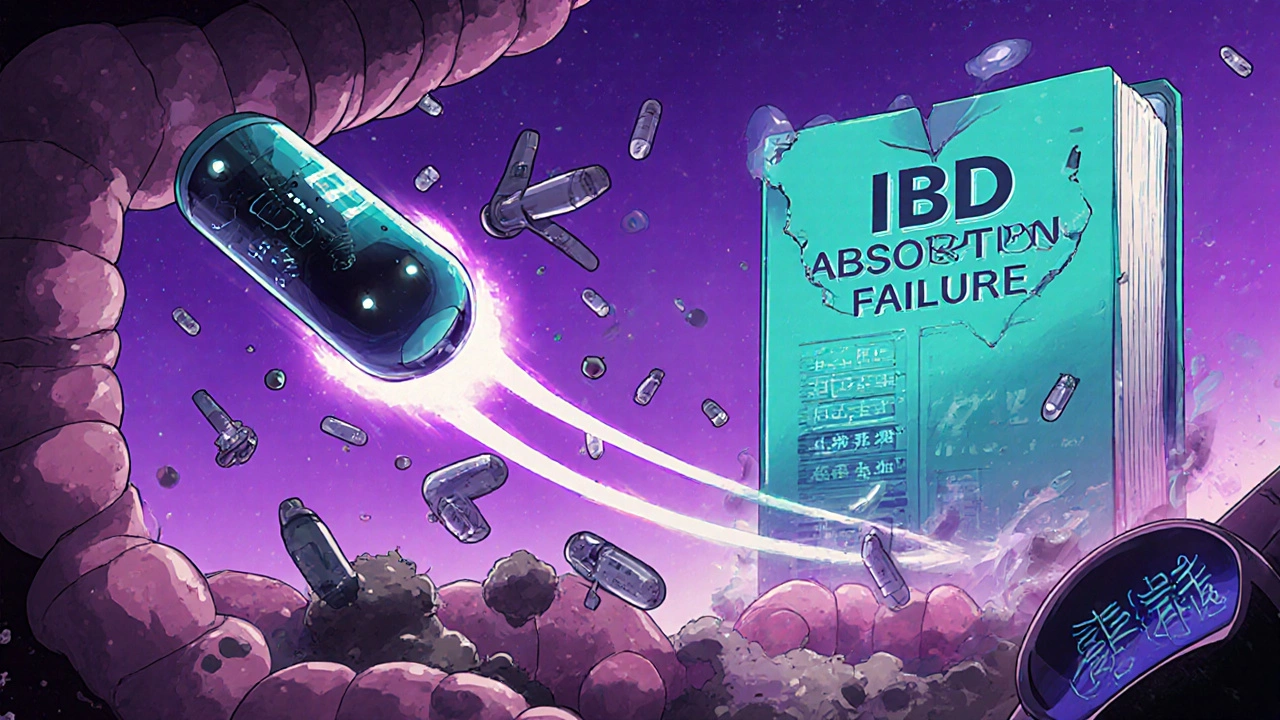
What You Can Do
If you’re on multiple GI meds and feel like nothing’s working, here’s what to check:- Are you taking your meds on an empty stomach when required? (Levothyroxine, tetracycline, bisphosphonates)
- Are you spacing out your fiber supplements? Take them 2-3 hours apart from other meds.
- Are you using antacids or PPIs? They can interfere with absorption of many drugs.
- Do you have diarrhea or constipation? That changes transit time. Talk to your doctor about adjusting timing or dosage.
- Are you on a GLP-1 agonist? Be extra careful with narrow-therapeutic-index drugs.
- Ask your pharmacist: Is there a liquid, chewable, or extended-release version that might work better for you?
The Bigger Picture
The pharmaceutical industry is waking up. Companies are now building disease-state models into drug development. The FDA and EMA have issued new guidance on testing drugs in patients with IBD, not just healthy volunteers. In vitro gut simulators now match clinical data 85-90% of the time. And there are early trials using smart capsules with pH and pressure sensors to track how a drug moves through your gut in real time. But here’s the truth: most doctors aren’t trained to think about absorption. Drug labels rarely mention IBD, short bowel, or gastroparesis. That’s why patients suffer in silence. You might be taking the right drug, at the right dose-but your gut just won’t let it in. The solution isn’t just more pills. It’s smarter formulations, better testing, and more awareness. Until then, if your meds aren’t working, it might not be your fault. It might just be your gut.Why do some GI medications stop working even if I take them the same way every day?
Your gut isn’t static. Inflammation, motility changes, food intake, and even stress can alter how drugs are absorbed. For example, someone with Crohn’s disease may have a flare-up that flattens intestinal villi, cutting absorption by 40%. Even if you take your pill at the same time, the physical environment inside your gut has changed. That’s why drug levels can swing unpredictably-especially with medications like mesalamine or warfarin.
Can food really make a difference in how well a pill works?
Absolutely. Fatty meals can delay gastric emptying by 2-4 hours, which means your pill sits in your stomach longer instead of moving to the small intestine where most absorption happens. For drugs like levothyroxine or certain antibiotics, this can reduce absorption by up to 50%. Even a high-fiber breakfast can trap drugs in the gut. Always follow the label: "take on empty stomach" means no food for at least 30-60 minutes before and after.
Why do some generic versions of my GI medication not work as well?
Generic drugs must contain the same active ingredient, but they don’t have to match the exact formulation. The salt form, crystal structure, or coating can be different. For drugs with poor solubility-like griseofulvin or some antifungals-this changes how fast the drug dissolves. If it dissolves too slowly, it passes through your gut before being absorbed. That’s why some people notice a drop in effectiveness after switching generics. Talk to your pharmacist about sticking with the brand if you’ve had consistent results.
Are there new types of GI medications that absorb better?
Yes. New formulations use nanoparticles, liposomes, or absorption enhancers like sodium caprate to help drugs cross the intestinal barrier. These can boost bioavailability by 2-3 times for poorly soluble drugs. Some are already on the market for cancer drugs and vitamins. For GI conditions, delayed-release and targeted-release versions (like Asacol HD or Lialda) are designed to release drug only in the colon, avoiding stomach acid. But these are still the exception-only 15-20% of oral drugs have special labeling for IBD patients.
Should I ask for blood tests to check if my GI meds are working?
If you’re on a drug with a narrow therapeutic window-like warfarin, digoxin, phenytoin, or immunosuppressants-yes. For others, like thyroid meds or antibiotics, therapeutic drug monitoring isn’t routine, but it can still help. If you’re experiencing symptoms despite taking your dose, ask your doctor about checking blood levels. Many patients with IBD or short bowel syndrome have undetectable drug levels despite perfect adherence. Testing can reveal absorption problems before complications arise.
What should I do if my doctor says my meds are fine but I still feel awful?
Trust your experience. If you’re taking your meds correctly and still having symptoms, the issue might be absorption. Ask for a referral to a clinical pharmacist who specializes in GI disorders. They’re trained to spot drug-gut interactions, adjust formulations, and coordinate with your gastroenterologist. Also, check if your medication has a liquid, chewable, or extended-release alternative. Sometimes, switching delivery methods makes all the difference.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.