When you pick up a prescription, most people assume the pharmacist is just filling a bottle. But if you’re on multiple medications-especially if cost is a concern-there’s a much bigger job happening behind the counter. That’s where medication therapy management comes in. It’s not just about counting pills. It’s about making sure every pill you take is the right one, at the right dose, for the right reason-and that you can actually afford it.
What Medication Therapy Management Really Means
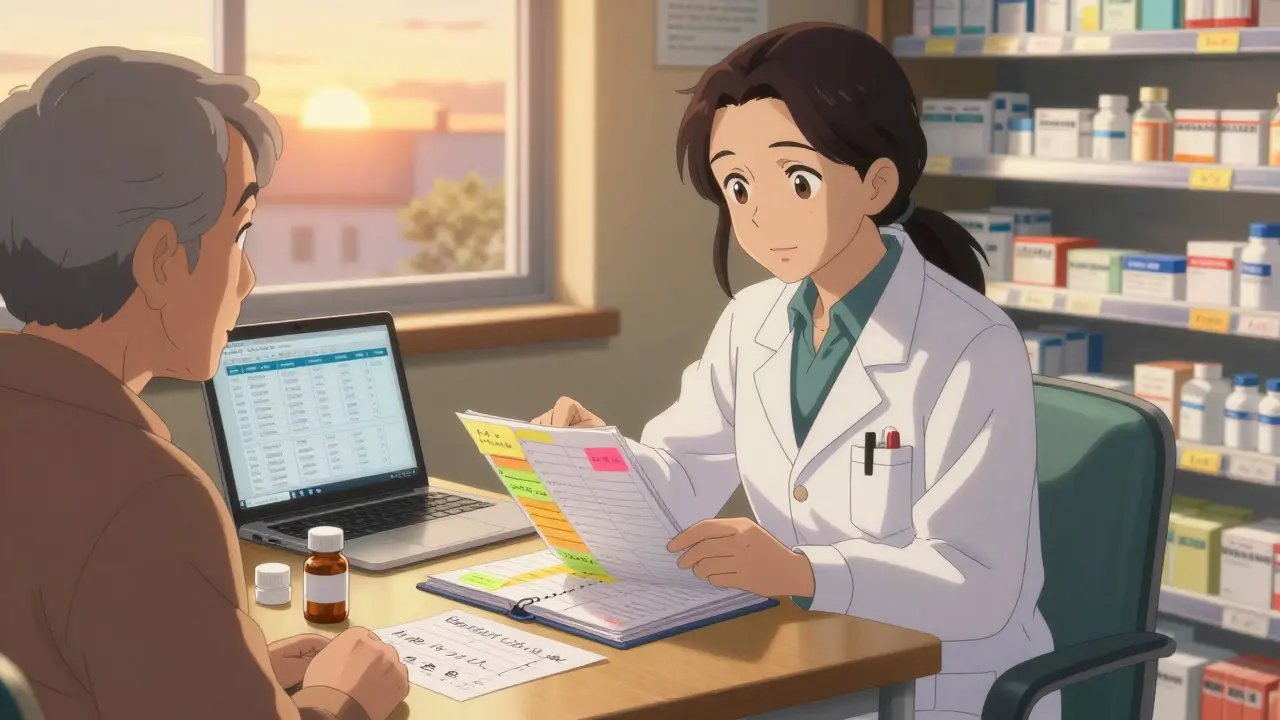
Medication Therapy Management, or MTM, is a structured service where pharmacists sit down with patients to review every medication they’re taking-prescription, over-the-counter, supplements, even herbal remedies. The goal? To fix problems before they become emergencies. This isn’t a quick chat at the pickup window. A full MTM session lasts 20 to 40 minutes. Pharmacists look at drug interactions, duplicate therapies, side effects, and whether the meds even make sense for the patient’s condition. The Centers for Medicare & Medicaid Services (CMS) has required all Medicare Part D plans to offer MTM since 2006. That’s because the data doesn’t lie: when pharmacists run these reviews, hospital readmissions drop by 23% within 30 days. Medication errors fall by 61%. And patients stick with their meds 18.7% more often.The Generic Drug Advantage
Here’s where pharmacists make a real difference-especially with generic drugs. The FDA says generics are chemically identical to their brand-name versions. They have the same active ingredient, same dosage, same safety profile. The only difference? Price. Generics cost 80% to 85% less. For a patient taking five chronic medications, that’s hundreds of dollars a month saved. But many patients still hesitate. They think, “If it’s cheaper, it must be weaker.” That’s a myth. Pharmacists in MTM sessions spend time debunking this. They show patients the FDA’s Orange Book ratings-A-rated generics are fully equivalent. Even for tricky drugs like warfarin or levothyroxine, where narrow therapeutic windows matter, pharmacists check bioequivalence data and monitor labs closely after switching. One HealthPartners study found that when pharmacists proactively recommended generic switches during MTM visits, patients saved 32% on their total drug costs. Another patient on Reddit shared how her $400/month brand-name inhaler was switched to a $15 generic. She cried-not from sadness, but relief. She could finally afford groceries and meds without choosing between them.How Pharmacists Decide When to Switch
Not every brand can or should be swapped. Pharmacists don’t just pick the cheapest option. They use tools like the Medication Appropriateness Index (MAI), which scores drugs across 10 criteria: is it indicated? Is it effective? Is the dose right? Is it cost-effective? For example, if a patient is on a brand-name statin and their cholesterol is under control, but they’re paying $120 a month, the pharmacist checks the Orange Book. If there’s an A-rated generic available for $12, they recommend the switch-then follow up in two weeks to check for side effects or concerns. They also look at refill patterns. If someone skips doses because the copay is too high, that’s a red flag. A pharmacist might find a generic alternative, suggest a 90-day supply through mail-order (often cheaper), or connect them with manufacturer assistance programs. In one APhA Foundation survey, 68% of MTM participants saw their out-of-pocket costs drop-on average, by $214 a month.
Why MTM Is Different from Regular Pharmacy Service
Traditional pharmacy work is transactional. A patient walks in, the pharmacist dispenses the script, checks for interactions in seconds, and moves on. Average interaction time? About 1.7 minutes. MTM is proactive. Pharmacists dig deeper. They ask: “What’s your biggest concern about your meds?” “Do you ever skip doses because of cost?” “Are you taking anything else your doctor doesn’t know about?” In a single Comprehensive Medication Review, pharmacists identify an average of 4.2 medication-related problems. That’s not one or two-four or more. Maybe the patient is on two blood pressure drugs that do the same thing. Maybe they’re taking a statin that interacts with grapefruit juice. Maybe their diabetes med is causing low blood sugar because they’ve lost weight and haven’t told their doctor. These aren’t mistakes by doctors. They’re gaps in communication. And pharmacists are the only providers trained to see them across the whole medication picture.Barriers to Getting MTM Services
Despite the proven benefits, MTM isn’t as widespread as it should be. Only 15% to 25% of eligible Medicare beneficiaries actually use the service. Why? Most don’t know it exists. Others are told by their pharmacy, “We don’t offer it.” The real issue? Reimbursement. Medicare pays $50 to $150 per MTM session. But commercial insurers? They pay $25 to $75. For a pharmacist spending 40 minutes on a patient, plus 10 to 15 minutes documenting it, that’s barely above minimum wage. Many pharmacies can’t afford to offer it without financial support. Another hurdle? Paperwork. MTM requires SOAP notes (Subjective, Objective, Assessment, Plan), electronic documentation, and communication with prescribers. Only 38% of community pharmacies have seamless integration with electronic health records. Without that, the process becomes too slow. And state laws vary. Only 42 states have clear rules letting pharmacists practice MTM independently. In the rest, they need a collaborative agreement with a doctor-which takes time and legal work.
What’s Changing in 2025
The tide is turning. Telehealth has made MTM more accessible. Since the pandemic, 63% of MTM programs now offer virtual visits. Patients can do their review from their living room. New tools are emerging too. Some pharmacists now use pharmacogenomic testing-checking a patient’s DNA to see how they metabolize drugs. That helps decide whether a generic is truly the best fit. For example, someone with a CYP2C19 gene variant might not break down clopidogrel properly. Switching to a generic version of a different drug could be safer than sticking with a brand. The American Pharmacists Association is pushing for standardized reporting on generic substitution outcomes. By 2025, MTM programs will track not just how many switches happened, but how many patients stayed on therapy, how many ER visits dropped, and how much money was saved. Meanwhile, the Pharmacist Medicare Benefits Act-though not yet passed by the Senate-could expand access to 38 million more Americans if it becomes law. That would mean direct Medicare reimbursement for pharmacists, not just through Part D plans.What Patients Should Do
If you’re on three or more chronic medications, or you’re struggling to pay for your prescriptions, ask your pharmacist: “Do you offer Medication Therapy Management?” Don’t wait for them to come to you. Most won’t unless you ask. You can also call your Medicare Part D plan directly-they’re required to notify you if you qualify. You don’t need a doctor’s referral. Bring a list of everything you take-including vitamins, supplements, and over-the-counter meds. Be honest about cost issues. Say: “I skipped my last refill because I couldn’t afford it.” That’s the kind of info that changes outcomes. And if your pharmacist recommends a generic-ask why. They should be able to explain the FDA rating, the cost difference, and how it compares to your current med. If they can’t, it’s time to find one who can.Why This Matters
Medication therapy management isn’t a luxury. It’s a lifeline. For patients juggling diabetes, heart disease, and depression meds, the right pharmacist can mean the difference between getting better and getting worse. Generics aren’t just cheaper-they’re often the only way people can stay on life-saving treatment. Pharmacists are trained to make those switches safely. They’re the only healthcare providers whose entire education is built around understanding how drugs work, interact, and cost. The system isn’t perfect. Reimbursement is broken. Awareness is low. But the data is clear: when pharmacists lead MTM, patients live longer, spend less, and feel more in control. It’s time to stop seeing pharmacists as order-fillers. They’re medication experts. And in the age of rising drug costs, we need them more than ever.What is Medication Therapy Management (MTM)?
Medication Therapy Management (MTM) is a structured service provided by pharmacists to review all of a patient’s medications-prescription, over-the-counter, and supplements-to ensure they’re safe, effective, and affordable. The goal is to fix medication-related problems, improve adherence, and reduce healthcare costs. MTM includes comprehensive medication reviews, personalized action plans, and follow-up care.
Can pharmacists really switch my brand-name drugs to generics safely?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also meet strict bioequivalence standards. Pharmacists use the FDA’s Orange Book to confirm A-rated generics, which are therapeutically equivalent. For drugs with narrow therapeutic windows (like warfarin or levothyroxine), pharmacists monitor lab values after switching to ensure stability.
Why don’t all pharmacies offer MTM services?
The main reason is reimbursement. Medicare pays $50-$150 per MTM session, but commercial insurers often pay only $25-$75. With a session taking 30-45 minutes plus documentation, many pharmacies can’t afford to offer it without financial support. Limited electronic health record integration and state laws restricting pharmacist scope of practice also create barriers.
Who qualifies for MTM under Medicare Part D?
You qualify if you have multiple chronic conditions (like diabetes, heart disease, COPD), take at least eight Part D-covered medications, and your annual drug costs exceed a certain threshold-usually over $5,000. Your plan must notify you if you’re eligible, but you can also call them directly to ask.
How much money can MTM save me on generics?
Patients in MTM programs save an average of $214 per month through generic substitutions and other cost-saving strategies. In some cases, like switching from a $400/month brand-name inhaler to a $15 generic, savings can exceed $4,500 a year. One study found that 37% of total cost savings in MTM came specifically from optimizing generic drug use.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.