When you’re sick, your body isn’t just fighting a cold or the flu-it’s fighting a battle with your blood sugar too. For people with diabetes, illness can turn a manageable day into a medical emergency. Fever, vomiting, or even a stuffy nose can spike blood glucose levels, sometimes to dangerous heights. The problem? Many people think if they’re not eating, they don’t need insulin. That’s a dangerous mistake. The real issue isn’t food-it’s stress hormones like cortisol and adrenaline, which surge during illness and make your body resist insulin. This can push blood sugar up by 30-50%, even if you’re barely eating anything. Left unchecked, this leads to diabetic ketoacidosis (DKA), a life-threatening condition that sends over 27% of diabetes-related hospitalizations to the ER, according to CDC data from 2022.
Never Skip Your Basal Insulin
Your long-acting insulin-whether it’s Lantus, Levemir, Basaglar, or another brand-is your safety net. Even if you’re too sick to eat, you still need it. Skipping it is one of the most common reasons people end up in the hospital with DKA. Your body still needs insulin to stop fat from breaking down into ketones. Without it, your blood becomes acidic, your organs start to shut down, and your life is at risk. The American Diabetes Association and the International Diabetes Federation both agree: never stop your basal insulin, no matter how bad you feel. If you’re on an insulin pump, don’t turn it off. If you’re on injections, keep giving your usual dose. In fact, during illness, you might need more. Many experts recommend increasing your basal rate by 20% for 12 hours if ketones are moderate or large. This isn’t guesswork-it’s based on decades of clinical observation. Your body is under stress. It needs extra insulin to keep up.Check Your Blood Sugar Every Few Hours
When you’re healthy, checking your blood sugar twice a day might be enough. When you’re sick, you need to check it every 2-3 hours if you’re a child, and every 3-4 hours if you’re an adult. Why so often? Because your numbers can swing wildly. One hour you’re at 150 mg/dL, the next you’re at 300 mg/dL. Don’t wait until you feel worse to check. Set alarms. Write it down. Use your CGM if you have one. Look for patterns: if more than half your readings over 12 hours are above 250 mg/dL, that’s a red flag. If your blood sugar hits 240 mg/dL or higher, it’s time to test for ketones. If you’re on insulin, ketone checks aren’t optional-they’re essential. If you’re on oral meds only, you still need to check ketones if your blood sugar stays above 240 mg/dL for more than a day. Urine strips are common, but they’re outdated. Blood ketone meters are faster, more accurate, and show real-time changes. A reading above 1.5 mmol/L means you need to act immediately. Don’t wait until you’re dizzy or vomiting. That’s too late.Hydration Is Your Lifeline
When your blood sugar is high, your body pulls water out of your cells to flush out the extra glucose through urine. That’s why you feel thirsty. But thirst isn’t enough-you need to drink on purpose. Dehydration makes everything worse. It thickens your blood, raises your blood sugar even more, and makes ketones build up faster. Adults should aim for 6-8 ounces of fluid every hour. For kids, the rule is simple: take their age in years and give them that many ounces per hour. A 10-year-old needs 10 ounces every hour. But not all fluids are the same. If your blood sugar is above 180 mg/dL, stick to sugar-free drinks: water, unsweetened tea, or sugar-free electrolyte solutions. If it’s between 100 and 180 mg/dL, mix half sugary fluid with half water. A 4-ounce serving of regular Gatorade or apple juice gives you 15 grams of carbs-just enough to prevent low blood sugar without spiking it too high. If your blood sugar drops below 100 mg/dL, switch to full-sugar fluids to keep your levels stable. The goal isn’t to drink a gallon-it’s to drink consistently. Keep a measuring cup handy. Sip every 15-20 minutes. If you can’t keep fluids down for more than 4 hours, call your doctor. Vomiting and dehydration are a deadly combo.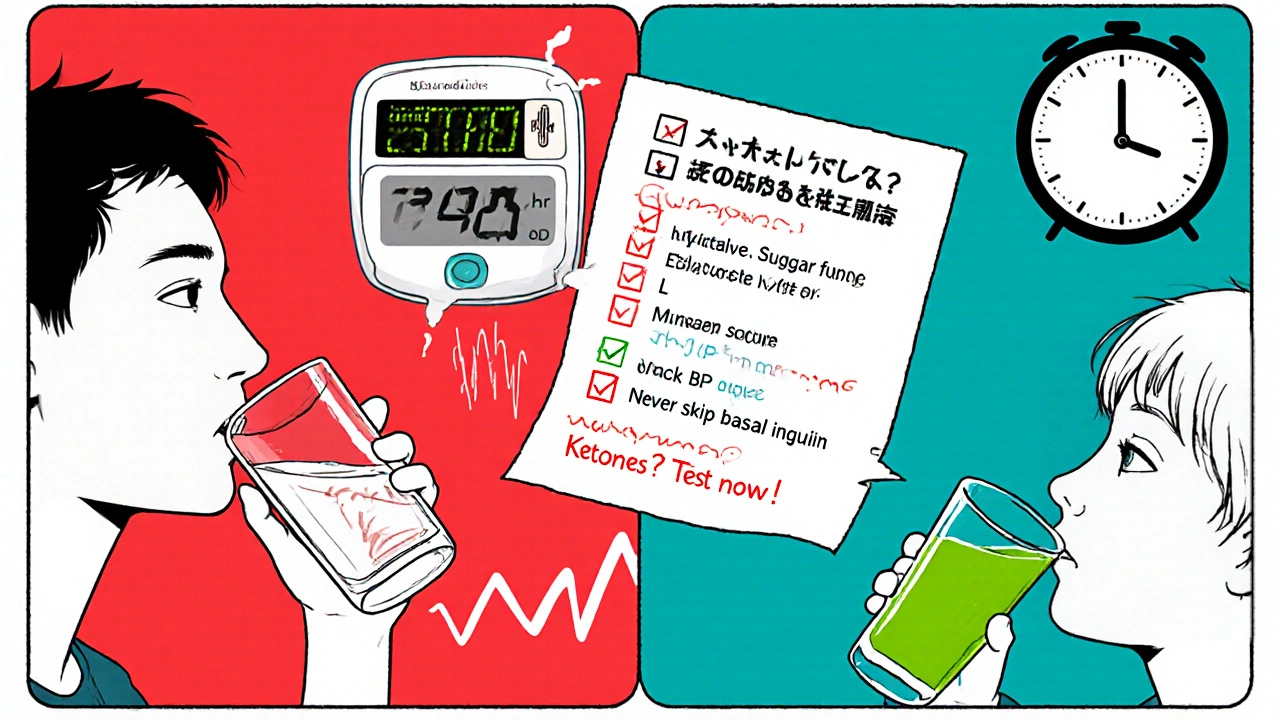
What to Eat When You Can’t Eat
You don’t need to force down a full meal, but you do need to keep some carbs coming. Your brain needs glucose-even when you’re sick. Skip carbs entirely, and your body starts breaking down fat for energy, which makes ketones. Aim for 15 grams of carbohydrates every hour if you can’t eat solid food. Easy options: 4 ounces of regular soda, 1/2 cup of applesauce, 1/2 cup of regular gelatin, or 1 tablespoon of honey. If you’re feeling nauseous, try sucking on ice chips made from sugar-free or sugary drinks, depending on your blood sugar. For adults, aim for 50 grams of carbs every 3-4 hours. That’s about 3-4 servings of 15 grams. Don’t worry about protein or fat right now. Focus on simple carbs that are easy to digest. If you’re on an insulin pump, you’ll need to give correction doses for high blood sugar, even if you’re not eating. If you’re on injections, use your usual insulin-to-carb ratio. Your body still responds to insulin-even when you’re sick.Type 1 vs. Type 2: Different Rules, Same Goal
Type 1 and Type 2 diabetes handle illness differently. If you have Type 1, you’re at higher risk for DKA because your body makes zero insulin. You must check ketones every time your blood sugar is over 240 mg/dL. You can’t skip insulin. Ever. Type 2 patients on insulin need to follow the same rules. But if you’re on pills only-like metformin or GLP-1 agonists-you may not need to check ketones unless your blood sugar stays above 240 mg/dL for over 12 hours. Still, you need to monitor closely. Some Type 2 patients actually need to start insulin temporarily during serious illness because their bodies can’t handle the stress. Don’t assume you’re “safe” just because you don’t take insulin daily. Illness can change everything. Also, your blood sugar target during sickness should be looser: aim for 110-180 mg/dL, not your usual tight range. This isn’t laziness-it’s safety. Low blood sugar during illness is just as dangerous as high blood sugar.What’s in Your Sick Day Kit?
Don’t wait until you’re sick to prepare. Build a sick day kit now. Here’s what you need: a 7-day supply of all your medications, unopened ketone test strips (they expire 6 months after opening), a blood ketone meter with extra batteries, a measuring cup, sugar-free and sugary fluids, easy-to-digest carbs (gelatin, applesauce, juice boxes), and a list of emergency contacts. Keep your insulin in a cool, dry place. Write down your usual insulin doses, your correction factors, and your doctor’s number. Store it in your fridge or a drawer you can find fast. Check your kit every 3 months. Expired strips give false negatives. That’s how people end up in the ER thinking they’re fine when they’re not. The FDA found that 18% of home ketone tests using expired strips gave wrong results. Don’t risk it.
When to Call for Help
You don’t have to figure this out alone. Call your doctor or go to the ER if: your blood sugar stays above 240 mg/dL for more than 24 hours; you have moderate or large ketones for more than 6 hours; you’re vomiting and can’t keep fluids down for 4 hours; you’re confused, breathing fast, or smell fruity on your breath; or you’ve lost more than 5 pounds without trying. These are signs your body is in crisis. The CDC says weight loss during illness is a major red flag. It means your body is burning fat and muscle because it has no insulin to use glucose. Don’t wait for symptoms to get worse. Call early. The ADA’s 24/7 helpline (1-800-DIABETES) handles over 12,000 sick-day calls a month. They can walk you through what to do next. Most calls are resolved in under 10 minutes.Common Mistakes and Real Stories
People make the same mistakes over and over. Skipping insulin because they’re not eating. Waiting too long to check ketones. Using expired strips. Drinking sugary drinks when blood sugar is already high. Ignoring dehydration. Reddit users share real stories: one dad said his son vomited everything he tried to drink during stomach flu and ended up in the ER for IV fluids. Another person said different doctors told him conflicting advice-some said to skip insulin, others said never to stop. He ended up in DKA with ketones at 22 mmol/L. That’s a life-threatening level. On the flip side, someone using a pump followed the +20% basal rate rule during the flu and kept their blood sugar between 150-200 mg/dL without any complications. The difference? Preparation and knowing the rules.What’s Next for Sick Day Management?
The field is changing. Newer closed-loop insulin systems automatically pause insulin when blood sugar drops, but they don’t yet know how to adjust for illness. That’s a gap. Experts are working on AI tools that predict when someone with diabetes is about to get sick based on early symptoms-like slight fatigue or changes in sleep-and suggest adjustments before blood sugar spikes. The NIH is funding this research, with tools expected by late 2025. For now, stick to the proven rules: check often, never skip insulin, hydrate constantly, test ketones, and call for help when something feels off. These aren’t suggestions-they’re survival steps.Can I skip my insulin if I’m not eating because I’m sick?
No. Even if you’re not eating, your body still needs insulin. Illness triggers stress hormones that raise blood sugar and cause your body to break down fat into ketones. Skipping insulin, even for a day, can lead to diabetic ketoacidosis (DKA), which is life-threatening. Keep your basal insulin on schedule. You may even need to increase it by 20% if ketones are present.
How often should I check my blood sugar when I’m sick?
Check every 2-3 hours if you’re a child, and every 3-4 hours if you’re an adult. Blood sugar can change rapidly during illness. Don’t wait until you feel worse. Set alarms. Use your CGM if you have one. If your readings stay above 240 mg/dL for more than 24 hours, or if over half your readings in 12 hours are above 250 mg/dL, test for ketones and contact your healthcare provider.
What fluids should I drink when I’m sick with diabetes?
Choose fluids based on your blood sugar. If it’s above 180 mg/dL, drink sugar-free fluids like water or sugar-free electrolyte drinks. If it’s between 100-180 mg/dL, mix half sugary fluid (like regular Gatorade) with half water. If it’s below 100 mg/dL, drink full-sugar fluids to prevent low blood sugar. Adults should aim for 6-8 ounces every hour. Kids should drink their age in ounces per hour (e.g., a 10-year-old drinks 10 ounces per hour). Sip slowly and consistently.
Do I need to check ketones if I have Type 2 diabetes?
If you take insulin, yes-check ketones anytime your blood sugar is above 240 mg/dL. If you’re on oral medications only, you don’t need to check ketones routinely unless your blood sugar stays above 240 mg/dL for more than 12 hours. Still, monitor closely. Illness can cause insulin resistance even in Type 2, and ketones can build up. If you’re unsure, check anyway. It’s better to be safe.
What should I do if I can’t keep fluids down?
If you’ve been vomiting or unable to keep liquids down for more than 4 hours, call your doctor or go to the ER. Dehydration and high blood sugar can quickly lead to DKA. You may need IV fluids and insulin to stabilize your condition. Don’t wait until you feel dizzy or confused. Early intervention saves lives.
Are urine ketone strips reliable?
They’re outdated and less accurate than blood ketone meters. Urine strips show ketones from hours ago, not what’s happening now. Blood ketone meters give real-time readings. A blood ketone level above 1.5 mmol/L means you need to act immediately. If you only have urine strips, use them-but treat moderate or large ketones the same way you would a blood ketone above 1.5 mmol/L. Replace expired strips-they can give false negatives.
Can over-the-counter cold medicines affect my blood sugar?
Yes. Many cough syrups, lozenges, and cold tablets contain sugar or alcohol, which can spike your blood sugar or interfere with medications. Always check labels. Look for sugar-free versions. If you’re unsure, ask your pharmacist. Even medicines labeled “diabetic-friendly” can contain hidden sugars. Keep track of anything you take and how it affects your numbers.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.