Imagine touching a light blanket and feeling like your skin is on fire. Or walking into a room with normal lighting and feeling like someone’s shining a spotlight in your eyes. This isn’t sensitivity-it’s pain that’s been turned up too high. That’s central sensitization-a real, measurable change in how your brain and spinal cord process pain signals, even when there’s no ongoing injury.
What Exactly Is Central Sensitization?
Central sensitization isn’t just "feeling more pain." It’s a biological rewiring. When nerves in your body send repeated or strong pain signals-like from an old injury, chronic inflammation, or even a viral infection-your spinal cord and brain start to change. Neurons become hyper-responsive. They start firing more easily, even to harmless touches. It’s like turning the volume knob on your pain system from 5 to 10, and then jamming it all the way up. This concept was first described by neuroscientist Clifford J. Woolf in 1983. He called it the "spinal cord wind-up phenomenon." Think of it like a doorbell that keeps ringing even after you’ve stopped pressing the button. The system gets stuck in overdrive. Today, we know this isn’t just a theory-it’s seen in brain scans, blood tests, and nerve response measurements. Up to 4% of people worldwide live with conditions where central sensitization is the main driver. Fibromyalgia is the most well-known example-around 90% of those diagnosed show clear signs. But it’s also behind many cases of chronic low back pain, long-lasting headaches, and even pain that lingers after surgery. The key clue? Pain that doesn’t match the injury. Pain that spreads. Pain that doesn’t go away when the tissue heals.How Your Nervous System Gets Stuck in Overdrive
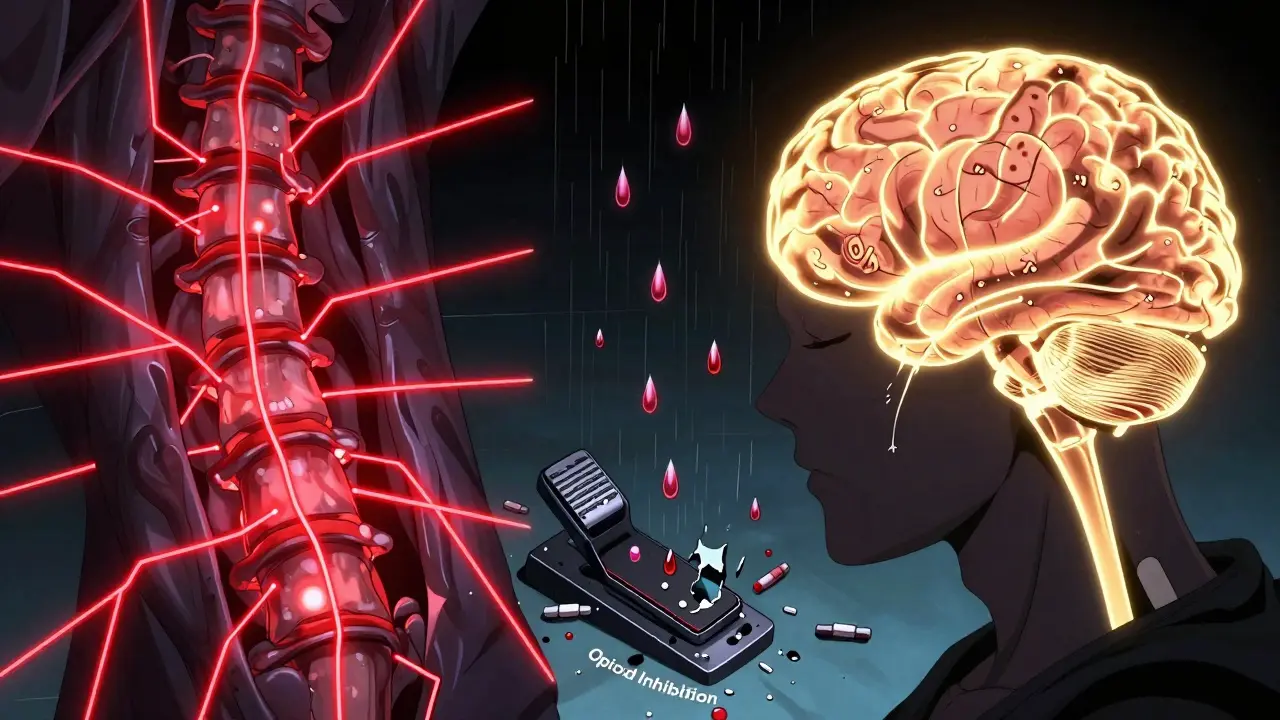
Your nervous system has two main ways of handling pain: sending signals up (excitatory) and putting the brakes on (inhibitory). In central sensitization, both systems go wrong. First, the "up" signals get stronger. Chemicals like substance P and glutamate flood the spinal cord. These are natural pain messengers, but in this state, they’re overproduced. Brain imaging shows pain-processing areas light up 20-35% more than normal when someone with central sensitization feels even mild discomfort. Second, the "brakes" fail. Your body naturally releases chemicals to calm pain signals. But in central sensitization, the opioid system-your body’s built-in painkillers-becomes less effective. Studies show mu-opioid receptor binding drops by 15-25%. That means your natural pain relief isn’t working like it should. Add to that: inflammation doesn’t just stay in the injured area. Immune cells in the nervous system get activated, releasing cytokines that keep the system stirred up. Stress hormones like norepinephrine rise by 25-40%. And your brain’s ability to filter out non-threatening sensations? It gets worse. This is why a light touch can feel like a burn, or why a quiet room feels unbearably loud.What Does It Feel Like? Real Symptoms
People with central sensitization don’t just have more pain-they have different pain. Here’s what it commonly looks like:- Widespread pain-not just in one spot, but across multiple areas: back, neck, legs, arms. In 95% of cases, pain isn’t limited to where the original injury was.
- Allodynia-pain from things that shouldn’t hurt. A shirt seam, a breeze, or a hug can feel painful. This happens in 85-90% of patients.
- Hyperalgesia-pain that’s way worse than it should be. A light poke feels like a pinch. A bump on the knee feels like a fracture.
- Temporal summation-repeated light touches build up into intense pain. This "wind-up" effect is seen in 70% of clinical tests.
- Brain fog-68% report trouble concentrating, memory lapses, or mental fatigue. This isn’t laziness-it’s your brain overloaded with pain signals.
- Sleep disruption-76% have sleep problems that go beyond just being woken by pain. Their nervous system never fully shuts down.
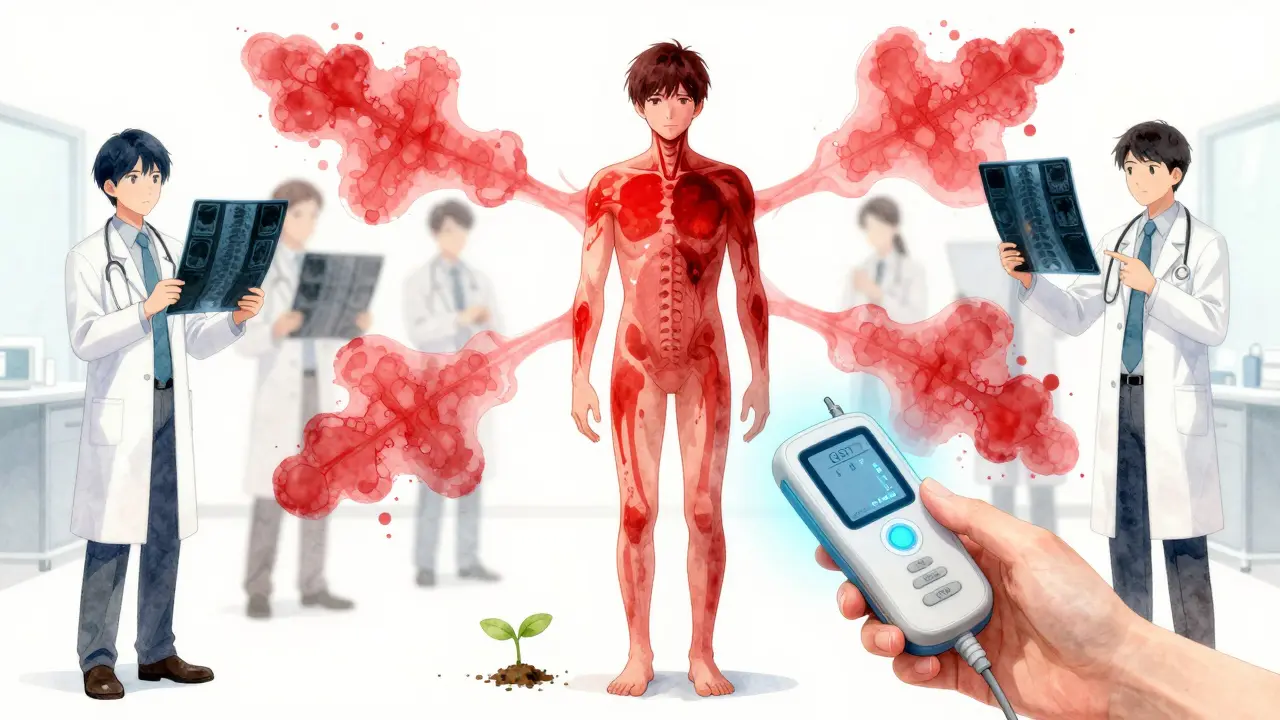
How Doctors Diagnose It
There’s no single blood test or X-ray for central sensitization. Diagnosis is based on patterns-and tools that measure how your nervous system responds. The most common method is quantitative sensory testing (QST). A technician applies controlled pressure, heat, or vibration to your skin and asks you to rate the pain. People with central sensitization report pain at much lower levels than others. Their pain threshold is often 20-30% lower. Another test is conditioned pain modulation. You’re exposed to a painful stimulus (like cold water) in one area, then asked to rate pain in another. Healthy people feel less pain because the body naturally inhibits it. In central sensitization, that inhibition drops by 40-50%. Your body loses its ability to put the brakes on. Pain drawings also help. People with nerve damage usually draw pain along specific nerve paths. People with central sensitization draw pain all over-like a full-body map. About 80% of cases show this non-anatomical pattern. The problem? Many doctors still look for structural damage-herniated discs, torn ligaments, arthritis. If they don’t see it on an MRI, they assume it’s "all in your head." But central sensitization is real. It’s just not visible on an X-ray. That’s why it takes most people 2-5 years and 4-6 doctors before they get the right diagnosis.How It’s Different From Other Types of Pain
Not all chronic pain is the same. Here’s how central sensitization stacks up:- Peripheral pain-like a sprained ankle-follows anatomy. Pain is where the injury is. It fades as tissue heals, usually within 6-12 weeks.
- Neuropathic pain-like diabetic nerve damage-follows nerve pathways. It’s often burning, tingling, or electric, and stays in one area.
- Central sensitization-spreads beyond the original site. Pain is disproportionate. It doesn’t follow nerves. It responds better to medications that target the brain and spinal cord.
How It’s Treated
You can’t fix central sensitization by just treating the original injury. You have to retrain the nervous system. Medications:- Pregabalin (Lyrica) and gabapentin calm overactive nerves. 300-1200mg daily helps 55% of people reduce pain by 30-50%.
- Duloxetine (Cymbalta) boosts serotonin and norepinephrine, helping the brain’s natural pain brakes. 60mg daily improves pain in 45% of users.
- Low-dose naltrexone (LDN) at 4.5mg nightly reduces inflammation in the nervous system. Studies show 25-35% improvement in fibromyalgia patients.
- Low-dose nortriptyline (25-50mg at night) helps with sleep and pain. 47% of patients report noticeable benefit.
- Graded exercise-start slow, increase by 10% per week. It doesn’t fix the injury, but it teaches your nervous system that movement isn’t dangerous. Functional improvement: 25-40%.
- Pain neuroscience education-learning how your nervous system works reduces fear. People who understand their pain report 20-30% less catastrophizing.
- Mindfulness and stress reduction-an 8-week program cuts pain interference by 25%. Stress fuels sensitization. Calming the mind helps calm the nerves.
Why This Matters
Central sensitization is no longer a fringe idea. It’s reshaping pain medicine. The NIH spent $63 million on research in 2023-up from $42 million in 2018. Academic pain centers now include central sensitization checks in 78% of cases, up from 45% just six years ago. But recognition varies. Rheumatologists spot it in 65% of fibromyalgia cases. Neurologists catch it in 55% of migraine patients. Orthopedic surgeons? Only 25%. That gap means many people are treated for the wrong problem-surgeries that don’t help, injections that fade, physical therapy that’s too aggressive. The future is promising. Researchers are developing biomarkers-like elevated substance P in spinal fluid or reduced opioid receptor binding seen on PET scans. New drugs targeting specific pain pathways are in Phase II trials. By 2027, diagnostic tools aim for 90% accuracy. Most importantly, understanding central sensitization removes the stigma. It’s not "all in your head." It’s in your nervous system. And that means it can be treated-not ignored, not dismissed, but understood and addressed.Is central sensitization the same as fibromyalgia?
No. Fibromyalgia is a diagnosis based on symptoms like widespread pain, fatigue, and sleep issues. Central sensitization is the underlying nerve mechanism causing those symptoms. About 90% of fibromyalgia patients have central sensitization, but not everyone with central sensitization has fibromyalgia. It can also drive chronic low back pain, TMJ disorders, and post-surgical pain.
Can central sensitization be reversed?
Yes. While it takes time, the nervous system is plastic-it can rewire. Removing ongoing triggers (like poor sleep, stress, or overexertion), using the right medications, and gradually reintroducing safe movement can reduce sensitivity. Many people see significant improvement within 6-12 months of consistent, targeted treatment.
Why do some doctors say it’s "all in my head"?
Because the pain isn’t visible on X-rays or MRIs, some doctors mistakenly think it’s psychological. But central sensitization is a real, measurable biological change. Brain scans show increased activity. Nerve tests show lowered pain thresholds. It’s not about being weak or imagining pain-it’s about your nervous system being stuck in high gear. The term "all in your head" is outdated and harmful.
Can stress make central sensitization worse?
Absolutely. Stress triggers the release of norepinephrine and cortisol, which directly activate pain pathways in the spinal cord. People with central sensitization are more sensitive to stress because their nervous system is already primed. Managing stress isn’t optional-it’s part of treatment.
Are there any new treatments on the horizon?
Yes. Five new drugs targeting specific pain receptors are in Phase II trials. Researchers are also testing wearable devices that use gentle electrical pulses to reset nerve sensitivity. And pain neuroscience education is now being integrated into physical therapy programs across Australia and the U.S., helping patients understand and manage their symptoms without relying solely on meds.


Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.