Medication-Citrus Interaction Checker
Check if Your Medication is Affected
Pomelo and Seville orange can dangerously interact with certain medications. Enter your medication name below to see if it's affected.
Most people know grapefruit can mess with their meds. But what about the big, pale pink fruit at the Asian market labeled "Chinese grapefruit"? Or the bitter orange marmalade your grandma swears by? These aren’t just exotic snacks-they’re silent drug disruptors. Pomelo and Seville orange behave just like grapefruit when it comes to medications, and in some cases, they’re even more powerful. If you’re on statins, blood pressure pills, or immunosuppressants, ignoring these fruits could put you in the hospital.
Why These Fruits Are More Dangerous Than You Think
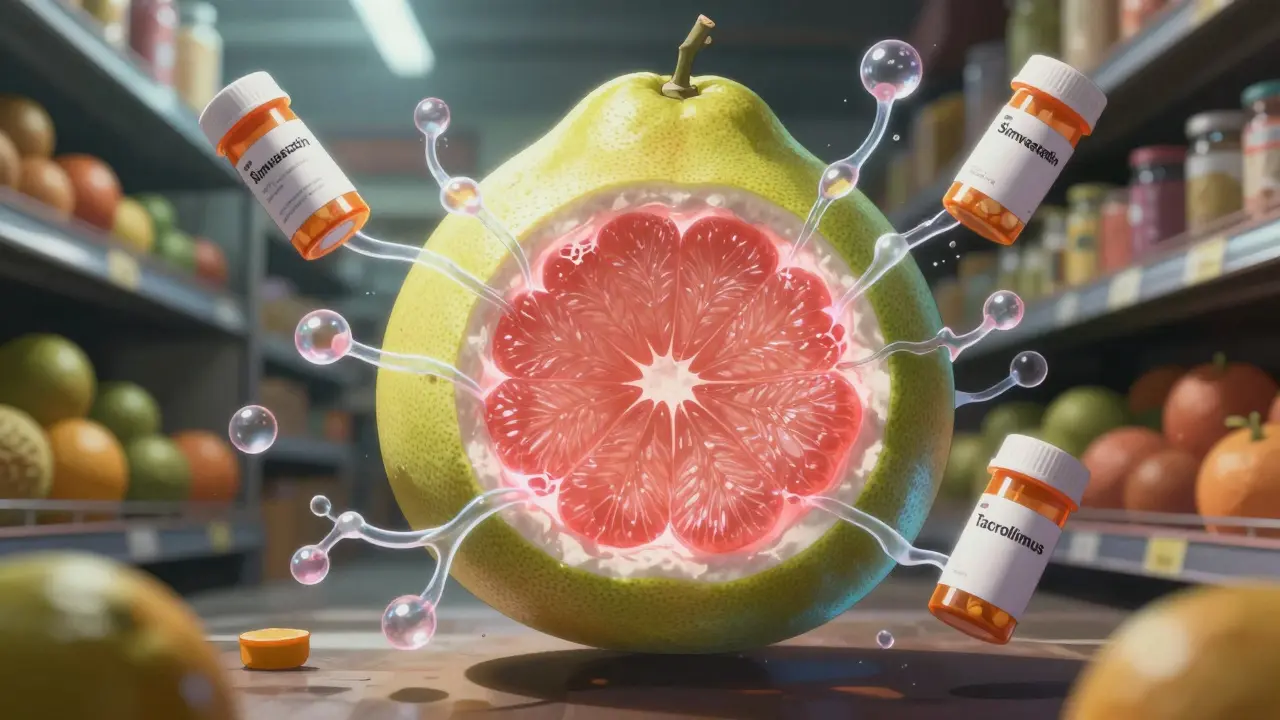
Pomelo and Seville orange don’t just look like grapefruit-they’re biochemically identical in the way they interfere with your body’s ability to process drugs. The culprits? Furanocoumarins, especially bergamottin and 6’,7’-dihydroxybergamottin. These compounds shut down an enzyme in your gut called CYP3A4, which normally breaks down drugs before they enter your bloodstream. When it’s blocked, your body absorbs way more of the medication than intended.
Here’s the kicker: pomelo often contains more of these compounds than grapefruit. Studies show pomelo juice can have up to 2.5 micromoles per liter of bergamottin, while grapefruit hovers around 1.0-2.0. Seville orange? Even higher. Some varieties hit 3.0-4.0 micromoles. That means a single glass of pomelo juice can boost the concentration of drugs like simvastatin by 350%-more than grapefruit does. In one documented case, a transplant patient taking tacrolimus ended up in the ICU after eating Seville orange marmalade daily. Their drug levels spiked 400%.
It’s not just juice. The peel, pulp, and even zest contain these inhibitors. That’s why marmalade is especially risky-it’s concentrated. One tablespoon of Seville orange marmalade can pack the same punch as a full glass of juice.
What Medications Are at Risk?
Not all drugs are affected. The danger is limited to medications metabolized by CYP3A4 and transported by OATP proteins. If your pill falls into one of these categories, you need to steer clear:
- Statins-simvastatin, lovastatin, atorvastatin (risk of muscle breakdown, kidney failure)
- Calcium channel blockers-amlodipine, felodipine, nifedipine (risk of dangerous low blood pressure, dizziness)
- Immunosuppressants-tacrolimus, cyclosporine (risk of kidney damage, infection, toxicity)
- Anti-anxiety drugs-buspirone, midazolam (risk of excessive sedation, respiratory depression)
- Antiarrhythmics-amiodarone, dronedarone (risk of irregular heartbeat)
- Some antidepressants and antipsychotics-quetiapine, lurasidone
Drugs like lisinopril, metformin, or sertraline? Safe. They don’t rely on CYP3A4. But if you’re on even one of the high-risk meds, don’t assume grapefruit is the only problem. Pomelo and Seville orange are just as dangerous-and less likely to be flagged on your prescription label.
The Hidden Danger: Marmalade and Mislabeling
Here’s where things get messy. Most people know to avoid grapefruit juice. But how many realize that the orange marmalade on their toast is made from Seville oranges? Or that the giant fruit they bought at the grocery store is pomelo, not a weird grapefruit?
A 2022 FDA review found only 37% of pomelo and Seville orange products carry any warning about drug interactions. Compare that to 78% of grapefruit products. That gap is deadly. Patients aren’t warned by pharmacists. Labels don’t say anything. And because these fruits aren’t as common in the U.S. or Australia, many doctors don’t ask about them.
Reddit threads and patient forums are full of stories like this: a man on simvastatin ate pomelo daily for two weeks, then woke up with muscle pain so bad he couldn’t stand. He had rhabdomyolysis-muscle tissue breaking down, poisoning his kidneys. No one told him it wasn’t just grapefruit that was dangerous.
And don’t get fooled by names. Pomelo is often sold as "Chinese grapefruit," "shaddock," or "pummelo." Seville orange might be labeled "bitter orange," "marmalade orange," or just "orange" on a jar. If it’s sour, bitter, or has thick, pithy skin, be cautious.

How Long Does the Effect Last?
One sip won’t just hurt you today. Furanocoumarins permanently disable CYP3A4 enzymes in your gut. Your body has to grow new ones. That takes time.
Effects can last up to 72 hours after you eat or drink these fruits. That means if you have a pomelo smoothie on Monday, it’s still interfering with your meds on Thursday. So skipping grapefruit on the day you take your pill doesn’t cut it. You need to avoid these fruits entirely while on the medication-or at least for three full days before starting it.
The FDA recommends a minimum 3-day avoidance window. The Mayo Clinic and European Medicines Agency echo this. No exceptions. Not even a small slice.
What Should You Do?
If you’re on medication, here’s your action plan:
- Check your meds. Look up your prescription on the University of Florida’s Drug Interaction Checker or ask your pharmacist. If it’s on the list of CYP3A4 substrates, you’re at risk.
- Ask about citrus. Don’t just say, "Do I need to avoid grapefruit?" Say, "Do I need to avoid pomelo, Seville orange, or bitter orange?" Most pharmacists still don’t screen for these unless prompted.
- Read labels. If you buy marmalade, check the ingredients. "Seville orange" or "bitter orange" means danger. Sweet oranges (Valencia, navel) are safe.
- Switch to safe citrus. Sweet oranges, tangerines, and clementines don’t contain furanocoumarins. You can eat them without worry.
- Track your intake. If you’re unsure, keep a food log for a week. Note every citrus fruit you eat. Show it to your doctor or pharmacist.
And if you’re a caregiver or family member? Don’t assume the patient knows. Many elderly patients eat marmalade daily because it’s "always been part of breakfast." They don’t connect it to their heart pill or transplant meds. A simple conversation could prevent an emergency.
Why Is This Still Overlooked?
There’s a reason grapefruit gets all the attention. It’s been studied since 1989. Pomelo and Seville orange? Not so much. There are fewer than 15 clinical studies on them as of 2023. That means less awareness, less research, and less pressure on manufacturers to warn consumers.
Only 29% of major pharmacy chains have these fruits in their electronic drug interaction alerts. That’s a huge gap. Pharmacists rely on those systems. If the system doesn’t flag it, the pharmacist won’t know to warn you.
And here’s the real problem: underreporting. A 2021 study found only 30% of adverse events caused by pomelo or Seville orange are correctly linked to the fruit. Doctors think it’s a side effect of the drug, not a food interaction. Patients don’t mention what they ate. So the problem stays hidden.
What’s Changing?
Good news: things are starting to shift. The FDA proposed new labeling rules in 2023 that would require warnings on all furanocoumarin-containing citrus fruits-including pomelo and Seville orange. Implementation is expected by mid-2025.
The University of Washington just launched a $2.1 million NIH-funded study specifically on pomelo-drug interactions. The European Food Safety Authority already requires warnings in 17 EU countries. And awareness among pharmacists is slowly rising.
But until those changes happen, the responsibility falls on you. Don’t wait for a label. Don’t wait for your doctor to ask. If you’re on a high-risk medication, treat pomelo and Seville orange the same way you treat grapefruit: avoid them completely.
Final Warning
These aren’t "maybe" risks. They’re proven, documented, and potentially life-threatening. One patient died from kidney failure after eating pomelo while on a statin. Another had a heart attack after Seville orange marmalade spiked their blood pressure meds. These aren’t rare cases-they’re preventable.
There’s no benefit to taking the risk. You won’t get more nutrients from pomelo than from an orange. You won’t lose anything by switching to sweet citrus. But you could lose your health-or your life-by ignoring this.
When it comes to your meds, don’t guess. Don’t assume. Ask. Check. Avoid. Your body will thank you.
Can I eat sweet oranges if I’m on medication?
Yes. Sweet oranges like navel, Valencia, or blood oranges do not contain furanocoumarins and are safe to eat with most medications. They’re a great alternative to grapefruit, pomelo, or Seville orange.
Does cooking or juicing reduce the risk?
No. Furanocoumarins are heat-stable and don’t break down during cooking, juicing, or pasteurization. Marmalade, baked goods, and juice all carry the same risk. Only the fruit’s chemistry matters-not how it’s prepared.
How do I know if a fruit is pomelo or Seville orange?
Pomelo is large (up to 12 inches wide), has thick, soft skin, and pale pink or white flesh. It tastes sweeter than grapefruit but still has a bitter aftertaste. Seville orange is small, round, and bright orange with thick, bumpy skin. It’s extremely sour and rarely eaten raw-usually only found in marmalade or extracts. If it’s labeled "bitter orange" or "marmalade orange," avoid it.
Is it safe to eat these fruits if I take my medication at night?
No. The enzyme inhibition lasts up to 72 hours. Taking your pill at night doesn’t protect you if you ate pomelo in the morning. The interaction happens in your gut before the drug even enters your bloodstream. Timing doesn’t matter-avoidance does.
What should I do if I accidentally ate pomelo or Seville orange?
If you’re on a high-risk medication like a statin or immunosuppressant, contact your pharmacist or doctor immediately. Don’t wait for symptoms. If you experience unexplained muscle pain, extreme fatigue, dark urine, dizziness, or irregular heartbeat, seek emergency care. These could be signs of toxicity.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.