What Exactly Is Contact Allergens?
When your skin reacts badly to something you touched - like your watch, shampoo, or even your jeans - it’s often not just dryness or irritation. It could be allergic contact dermatitis, a delayed immune response triggered by specific chemicals called contact allergens. Unlike a quick rash from poison ivy, this reaction doesn’t show up right away. It can take 24 to 72 hours after contact for redness, itching, or blisters to appear. That’s why so many people are confused about what’s causing their flare-ups.
These allergens aren’t rare. They’re hiding in everyday products: perfumes in lotions, metals in jewelry, preservatives in makeup, and even rubber in gloves. The tricky part? You might have used the same product for years without issue, then suddenly your skin starts reacting. That’s because your immune system can become sensitized over time - it’s like your skin finally says, “Enough.”
How Patch Testing Works - Step by Step
There’s only one reliable way to find out what’s causing your skin reaction: patch testing. It’s not a needle, not a scratch, and not a blood test. It’s a slow, quiet process that lets your skin tell you what it’s allergic to.
Here’s how it works:
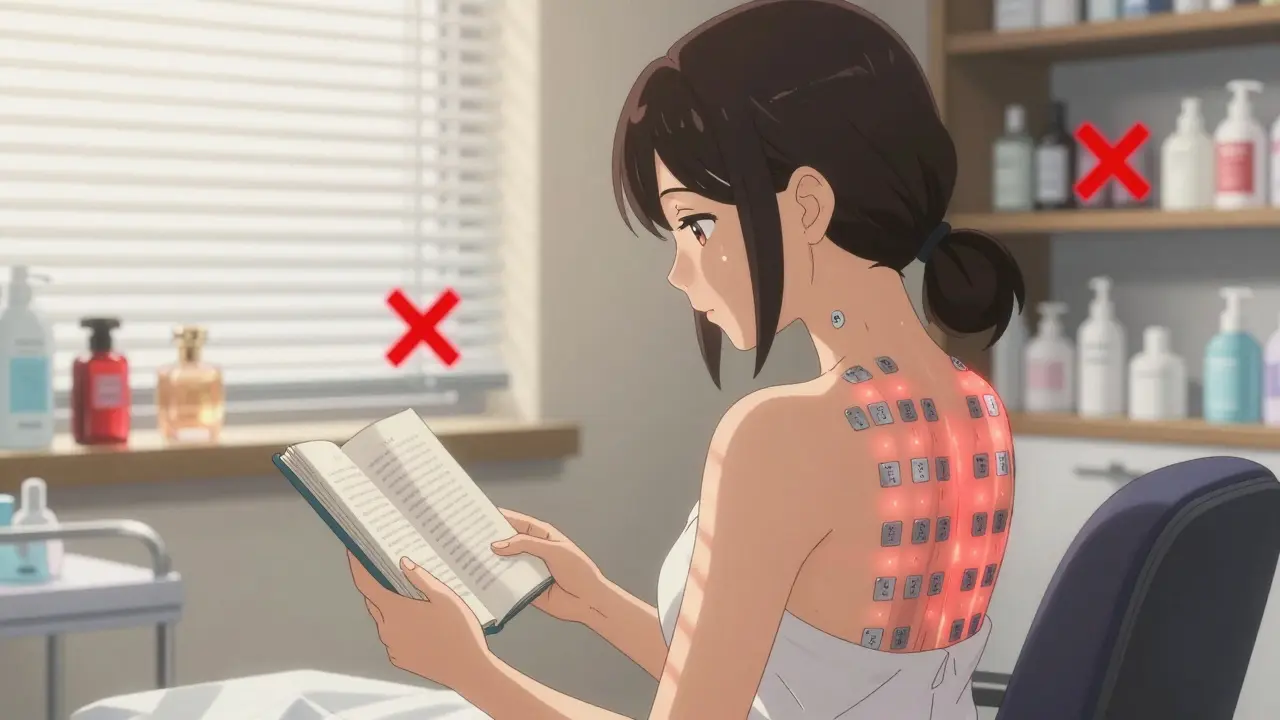
- On Monday, a dermatologist places small metal chambers (called Finn chambers) on your back. Each holds a tiny amount of a different chemical - anywhere from 30 to over 100 substances. These aren’t random. They’re standardized, high-purity allergens mixed with petrolatum to ensure accurate dosing.
- The patches stay on for exactly 48 hours. No showers, no sweating, no swimming. Moisture can wash away the allergens or cause false reactions. You’ll be given instructions to avoid strenuous activity and tight clothing that might rub the patches off.
- On Wednesday, the patches are removed. The dermatologist checks for early reactions - redness, swelling, or tiny blisters. But the real answer comes later.
- On Friday, you return for the final reading. Some reactions take up to 96 hours to show up. A positive result looks like a raised, red, itchy bump right where the patch was.
Unlike skin prick tests (which check for immediate allergies like pollen or peanuts), patch testing catches delayed reactions - the kind caused by your immune system slowly waking up to a substance you’ve touched repeatedly.
What’s in the Standard Patch Test Panel?
There’s no universal list, but most clinics in Australia and the U.S. use a baseline series that covers the most common culprits. These include:
- Nickel - found in jewelry, belt buckles, zippers, and even some cell phones. It’s the number one allergen worldwide.
- Chromium - in cement, leather tanning, and some paints. Construction workers and shoemakers often test positive.
- Formaldehyde - a preservative in makeup, shampoos, and baby wipes. Even “natural” products can contain it.
- Paraphenylenediamine (PPD) - the main ingredient in black hair dye. It’s a frequent cause of scalp and neck rashes.
- Coconut diethanolamide - a foaming agent in soaps and shampoos. Often mistaken for coconut allergy, but it’s not the oil - it’s the chemical.
- Neomycin - an antibiotic in first-aid creams. Ironically, it’s used to treat rashes but can cause them.
These 20-30 substances account for about 70% of all allergic contact dermatitis cases. But if your job or hobbies put you at risk - like being a florist (exposed to plants like chrysanthemums), a dental technician (methacrylates), or a nurse (latex, disinfectants) - your doctor might add an expanded panel. That bumps detection rates up to 80%.
Why Patch Testing Beats Guesswork
People often try to figure out their triggers by eliminating products one by one. It’s exhausting. You might stop using every new lotion, perfume, or detergent - only to still get a rash. Why? Because the culprit could be something you never thought of: the adhesive on your bandage, the fragrance in your laundry detergent, or even the nickel in your bra clasp.
Patch testing cuts through the noise. It doesn’t just tell you what to avoid - it tells you exactly what to avoid. One patient in Perth stopped getting hand rashes after years of trial and error. Her patch test showed a reaction to tert-butylhydroquinone, a preservative in her moisturizer. She’d been using it daily for five years. Once she switched, her skin cleared up in weeks.
And here’s something most people don’t know: you can still take antihistamines during patch testing. Unlike other allergy tests, antihistamines don’t interfere with the delayed immune response being measured. So if you’re on medication for eczema or hay fever, you don’t have to stop.
What Patch Testing Can’t Do
It’s not magic. There are over 3,000 known contact allergens. The standard panel only covers the most common ones. If your rash keeps coming back and your patch test is negative, it could be:
- Irritant contact dermatitis - caused by repeated exposure to soaps, detergents, or solvents. No immune system involved. Just damage from overuse.
- Photocontact dermatitis - a reaction that only happens when the allergen is on your skin and then exposed to sunlight.
- Uncommon allergens - like certain plant oils, industrial chemicals, or even new ingredients in skincare products.
In these cases, your dermatologist might suggest repeat open application testing. You apply the suspect product (like your favorite hand cream) to a small patch of skin on your forearm twice a day for 5-10 days. If a rash develops, you’ve found your trigger - without needing a formal patch test.
What Happens After a Positive Result?
Finding the allergen is only half the battle. The real win is avoiding it. But that’s easier said than done.
For example, if you’re allergic to nickel:
- Switch to stainless steel or titanium jewelry.
- Use clear nail polish on the backs of watch bands to create a barrier.
- Check labels on clothing - some zippers and buttons contain nickel.
If you react to fragrance: look for products labeled “fragrance-free,” not “unscented.” Unscented can still contain masking fragrances. Fragrance-free means no added scent at all.
For preservatives like formaldehyde or parabens, check ingredient lists. Many apps and websites now let you scan barcodes to check for allergens. Your dermatologist might also give you a list of safe brands.
And if your skin is already inflamed? Topical corticosteroids help calm the flare. For severe cases, short courses of oral steroids may be needed. Antihistamines won’t fix the rash - they just help with the itch.
When to Get Tested
You don’t need to wait until your skin is a mess. If you’ve had the same rash for more than two weeks, or if it keeps coming back in the same spot - especially after contact with something new - it’s time to ask about patch testing.
It’s also worth considering if:
- Your eczema doesn’t respond to standard treatments.
- You work with chemicals, cleaning products, or metals.
- You’ve had multiple skin reactions after using the same product.
Even if your rash seems mild, identifying the trigger can prevent long-term damage. Chronic scratching leads to thickened, cracked skin - a condition called lichenification. That’s harder to treat than the initial reaction.

Myths About Patch Testing
Let’s clear up some confusion:
- Myth: “I’m allergic to everything.”
Truth: You’re probably allergic to one or two. Patch testing finds them. - Myth: “It’s painful.”
Truth: It’s uncomfortable - you might feel a little itch or tightness - but it’s not painful. The patches are taped on, not injected. - Myth: “I can just use over-the-counter creams.”
Truth: Creams treat symptoms. Patch testing treats the cause. - Myth: “If I didn’t react last time, I’m safe.”
Truth: Sensitization can happen anytime. A product you used safely for years can suddenly trigger a reaction.
What’s Next for Patch Testing?
Scientists are constantly updating the allergen panels. As new ingredients appear in cosmetics and household products, dermatologists add them to tests. For example, methylisothiazolinone - once common in baby wipes - was added to panels after a surge in reactions in the 2010s.
There’s also growing interest in regional differences. In Australia, plant-based allergens like myroxylon (from balsam of Peru) are more common due to local plant exposure. In Europe, certain metal alloys are more prevalent in jewelry. Future panels will likely be more tailored to geography and lifestyle.
For now, patch testing remains the gold standard. No blood test, no app, no home kit can match its accuracy for identifying delayed allergic reactions.
Can patch testing cause a bad reaction?
Patch testing is designed to be safe. The allergens are diluted to levels that won’t cause severe reactions in most people. Some patients develop mild redness or itching at the test site - that’s the point. In rare cases, a strong reaction can cause blistering or scarring, especially if the patch is left on too long or if the patient has very sensitive skin. That’s why it’s always done under medical supervision. If you have active eczema on your back, your doctor may test on your arm instead.
How long does it take to see results after avoiding an allergen?
It varies. Some people notice improvement within days, especially if they’ve been exposed to the allergen daily. For others, it takes weeks - especially if the skin has been inflamed for a long time. Chronic rashes with thickened skin (lichenification) can take months to fully heal. The key is consistency. Even one accidental exposure can trigger a flare-up weeks later.
Is patch testing covered by insurance in Australia?
Yes, in most cases. Patch testing is considered a diagnostic procedure under Medicare. You’ll need a referral from your GP to a dermatologist. The cost varies by clinic, but the out-of-pocket expense is often minimal with Medicare rebates. Some private health insurers also cover part of the cost. Always check with your provider before scheduling.
Can children get patch tested?
Yes, but it’s less common. Children under 10 usually don’t get tested unless they have persistent, unexplained rashes that don’t respond to standard treatments. Their skin is more sensitive, and reactions can be harder to interpret. Dermatologists often start with simpler approaches, like elimination trials or repeat open application testing, before moving to formal patch testing.
What’s the difference between irritant and allergic contact dermatitis?
Irritant contact dermatitis happens when a substance directly damages your skin - like bleach, soap, or solvents. It doesn’t involve your immune system. Anyone can get it with enough exposure. Allergic contact dermatitis is different: it’s an immune response. You need to be sensitized first. It only affects people who are allergic, and it can happen after years of safe use. Patch testing only detects the allergic type.
Do I need to stop using all my skincare products before the test?
No. You should keep using your regular products up until the test. That way, the dermatologist sees what’s actually affecting your skin. But avoid applying anything to your back for at least 24 hours before the test. Also, don’t use topical steroids on your back for at least two weeks before the test - they can suppress reactions and give false negatives.
Final Thoughts: Knowledge Is Your Best Defense
Living with recurring skin rashes is frustrating. But you don’t have to guess anymore. Patch testing gives you real answers - not just temporary relief. Once you know what’s triggering your skin, you can make smart choices about the products you use, the clothes you wear, and even the tools you handle at work. It’s not just about avoiding rashes. It’s about taking back control of your skin - and your life.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.