Warfarin is one of the most commonly prescribed blood thinners in the world. It’s been around since the 1950s, and while newer drugs have taken over many uses, warfarin still plays a critical role - especially for people with mechanical heart valves or certain rare clotting disorders. But here’s the hard truth: warfarin doesn’t play nice with much of anything else. A single change in your diet, a new supplement, or even a common antibiotic can send your INR levels skyrocketing or crashing. And when that happens, you’re at serious risk - either of dangerous clots or uncontrolled bleeding.
How Warfarin Actually Works
Warfarin doesn’t thin your blood like water. Instead, it blocks vitamin K from doing its job. Vitamin K is what your body needs to make clotting factors - proteins that stop you from bleeding out after an injury. By slowing down this process, warfarin keeps your blood from clotting too easily. That’s good if you’re at risk for stroke or deep vein clots. But it’s dangerous if your body gets too much or too little of this effect.
The goal? Keep your INR between 2.0 and 3.0. That’s the sweet spot for most people. Go below 2.0? You’re at risk for clots. Above 3.0? You could bleed internally without even knowing it. And here’s the kicker: small changes in what you eat or take can shift your INR by 0.5 to 1.5 points in just a few days. That’s enough to land you in the ER.
Foods That Mess With Warfarin
The biggest food culprit? Vitamin K. It’s not that you have to avoid it entirely - you need vitamin K to live. But you need it consistent. A sudden spike or drop in vitamin K intake throws your INR off balance.
- High-vitamin K foods: Spinach (1 cup cooked = 145 mcg), kale (1 cup cooked = 1,062 mcg), broccoli (1 cup cooked = 220 mcg), Brussels sprouts, cabbage, parsley, and green tea.
- What to do: Eat about the same amount every day. If you normally have a salad with spinach twice a week, keep doing that. Don’t suddenly start eating kale every morning. Don’t quit greens cold turkey. Consistency matters more than quantity.
One patient I spoke with - a 68-year-old man from Perth - switched from eating white rice to brown rice for health reasons. Brown rice has more vitamin K. His INR dropped from 2.6 to 1.8 in four days. He almost had a stroke. He had to go back to white rice and increase his warfarin dose.
Other foods to watch:
- Alcohol: More than 1-2 drinks a day can increase bleeding risk. Three or more? That risk jumps over 3 times. It also messes with how your liver processes warfarin.
- Grapefruit: Not as strong as with some other drugs, but it can still interfere with how warfarin is broken down. Best to avoid large amounts.
- Fruit juice: Cranberry juice has been linked to INR spikes. The evidence isn’t 100% solid, but enough people have had problems that doctors recommend avoiding it.
Supplements That Can Kill You
People think supplements are harmless. They’re not. Especially not when you’re on warfarin.
- Vitamin E: High doses (over 400 IU/day) can thin your blood even more. It’s not just a “vitamin” - it acts like a blood thinner.
- Garlic: Garlic pills, garlic oil, raw garlic - all of them can increase bleeding risk. One study found people taking garlic supplements had INR levels rise above 4.0.
- Ginkgo biloba: Used for memory, but it also interferes with platelets. It’s a dangerous combo with warfarin.
- Green tea: Not just the leaves - supplements and extracts can drop your INR. One user reported her INR fell from 2.8 to 1.9 after taking green tea capsules for a month.
- St. John’s Wort: This herbal antidepressant speeds up how fast your liver breaks down warfarin. Result? Your blood clots too easily.
- Coenzyme Q10: It’s structurally similar to vitamin K. Some experts believe it may counteract warfarin’s effect.
A 2022 survey of 1,200 warfarin users found that 24% had a dangerous interaction from a supplement. Half of them didn’t even tell their doctor they were taking it.

Prescription Drugs That Change Everything
Here’s where things get scary. Hundreds of prescription drugs interact with warfarin. Some make it stronger. Some make it weaker. And many do it fast - within 48 hours.
Drugs that make warfarin stronger (higher INR, higher bleeding risk):
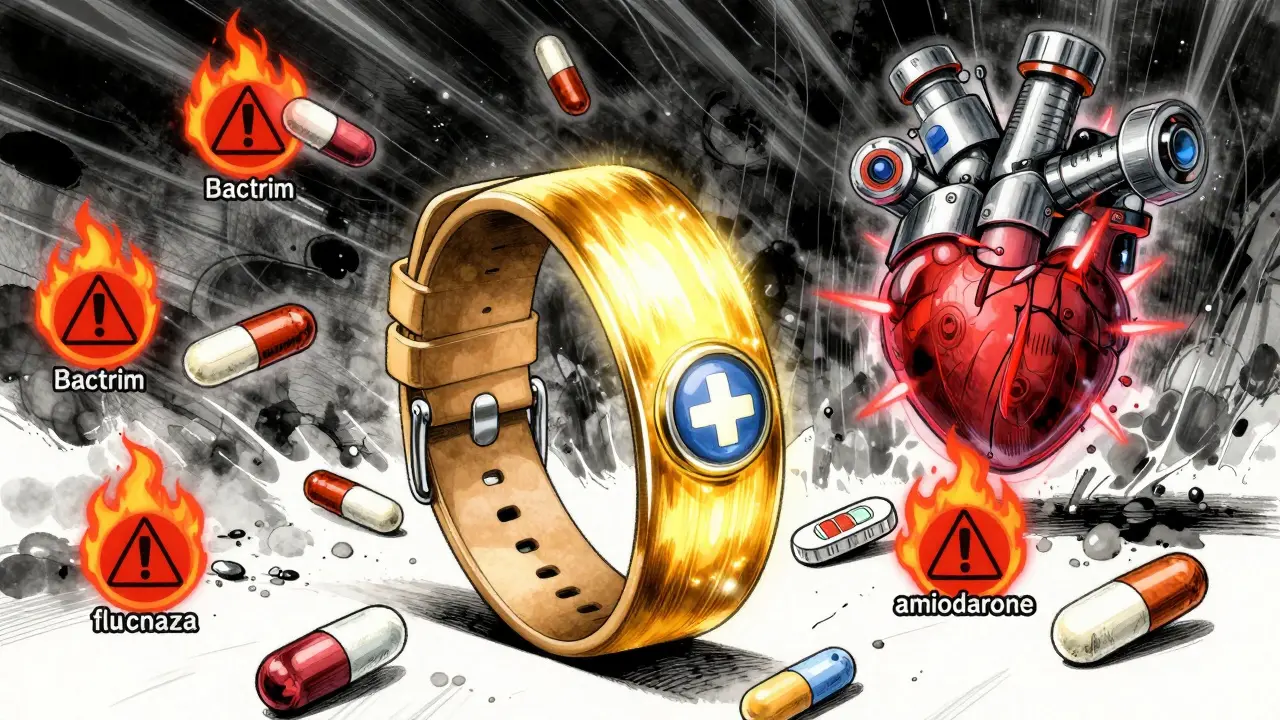
- Antibiotics: Especially trimethoprim-sulfamethoxazole (Bactrim), ciprofloxacin (Cipro), and metronidazole (Flagyl). These can spike your INR by 50-100%. One patient had to go to the ER three times after taking Bactrim for a UTI.
- Antifungals: Fluconazole (Diflucan) is a big one. It can double warfarin levels.
- Amiodarone: Used for heart rhythm problems. It’s notorious for causing dangerous INR spikes. Dose reductions of 30-50% are often needed.
- NSAIDs: Ibuprofen, naproxen, diclofenac - these aren’t just painkillers. They irritate your stomach lining and make bleeding more likely. Even a few days of use can be risky.
- SSRIs: Some antidepressants like fluoxetine (Prozac) and sertraline (Zoloft) can also increase bleeding risk.
Drugs that make warfarin weaker (lower INR, higher clot risk):
- St. John’s Wort: Already mentioned - but it’s a prescription drug too.
- Barbiturates: Used for seizures or sedation. Speed up warfarin breakdown.
- Rifampin: An antibiotic used for tuberculosis. It can cut warfarin’s effect in half.
Here’s the thing: your doctor doesn’t always know about every interaction. A 2021 review found that 84% of reported warfarin interactions came from single case studies - not solid science. But some are rock solid: Bactrim, fluconazole, amiodarone. Treat those like landmines.
Why Warfarin Still Matters
You might hear people say, “Just switch to Eliquis or Xarelto.” And for many, that’s true. DOACs (direct oral anticoagulants) don’t need regular blood tests, have fewer interactions, and are easier to manage.
But here’s why warfarin hasn’t disappeared:
- Mechanical heart valves: DOACs are dangerous here. Warfarin is still the only safe option.
- Severe kidney failure: If your kidneys are failing, DOACs can build up in your body. Warfarin doesn’t rely on kidney function.
- Cost: Warfarin costs $4-$10 a month. Eliquis? Over $500. For people on Medicare or without insurance, that’s life-changing.
- Reversibility: If you bleed badly, doctors can give you vitamin K or a clotting factor concentrate to reverse warfarin in hours. With DOACs, reversal is harder and more expensive.
So while fewer people are starting warfarin now, it’s still essential. And for those on it, managing interactions isn’t optional - it’s survival.
What You Should Do
Here’s the practical advice - no fluff.
- Get your INR checked regularly. Even if you feel fine. Stable? Still check every 4 weeks. Unstable? You might need it every week.
- Keep a food and supplement log. Write down what you eat, what pills you take, and when. Bring it to every appointment.
- Never start or stop a supplement without telling your doctor. Even “natural” ones.
- Use a drug interaction checker. The American Society of Hematology has a free online tool that lists over 297 interactions. Use it before taking anything new.
- Wear a medical alert bracelet. If you’re in an accident and unconscious, paramedics need to know you’re on warfarin.
- Know the signs of bleeding: Unusual bruising, pink or red urine, black or bloody stools, nosebleeds that won’t stop, headaches or dizziness (could mean brain bleed).
One of the most successful patients I’ve worked with eats exactly one cup of cooked spinach every night at 6 p.m. - no more, no less. She’s been stable for five years. That’s the power of consistency.
The Future of Warfarin
There’s new tech coming. In 2023, the FDA approved a genetic test called Warfarin GenAssist. It looks at two genes - CYP2C9 and VKORC1 - to predict how you’ll respond to warfarin. It can cut the time to stable dosing by over two weeks. It’s not perfect, but it helps.
AI is also stepping in. A 2023 study showed a machine learning model predicted the right warfarin dose 82% of the time - better than human doctors. But it’s not in clinics yet.
For now, the best tool you have is awareness. Knowledge. Consistency. And never, ever assuming a pill or food is “safe” just because it’s natural or over-the-counter.


Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.