Anticholinergic Burden Calculator
What is this tool?
This calculator helps you assess your cumulative anticholinergic burden from medications. Each medication is rated on the ACB Scale (0-3), where higher scores indicate greater anticholinergic effect. A score of 3 or higher is a red flag for increased dementia risk.
Important: This is for educational purposes only. Consult your healthcare provider before making any medication changes.
Added Medications
Your Total Anticholinergic Burden Score:
0What Your Score Means
0-2
Low risk. Continue monitoring your medications.
3-5
Medium risk. Consider discussing alternatives with your doctor.
6+
High risk. Consult your healthcare provider about safer alternatives.
Important Information
The American Geriatrics Society Beers Criteria recommends avoiding chronic use of first-generation antihistamines in older adults. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) have ACB scores of 0 or 1 and are safer alternatives.
Many older adults take antihistamines every day-not for allergies, but for sleep. A pill at bedtime seems harmless. But when that same person is also taking a bladder medication, a depression pill, or even an over-the-counter stomach remedy, something dangerous is building up quietly in their body. This isn’t just one bad drug. It’s the cumulative anticholinergic burden-the total effect of multiple medications that block acetylcholine, a key brain chemical needed for memory, focus, and muscle control.
What Is Anticholinergic Burden, Really?
Anticholinergic burden isn’t a buzzword. It’s a measurable risk. Every medication that blocks acetylcholine adds a point to your score. The most trusted tool to measure this is the ACB Scale, developed in 2008 by Dr. Malaz Boustani. It rates drugs from 0 (no effect) to 3 (strong effect). A score of 3 or higher in adults over 65 is a red flag. Studies show people with that score are 50% more likely to develop dementia over five years.First-generation antihistamines like diphenhydramine (Benadryl) and chlorpheniramine are rated 2 or 3 on the ACB scale. That’s the same level as oxybutynin (for overactive bladder) or amitriptyline (for depression). Even one of these drugs alone is risky. But when you stack them? The risk doesn’t just add up-it multiplies.
Why Antihistamines Are the Silent Culprit
Most people don’t realize antihistamines are anticholinergics. They think of them as allergy pills. But diphenhydramine is also in nighttime sleep aids, cold medicines, and even some stomach remedies. In 2022, 40% of adults over 65 in the U.S. were using these pills regularly-often for years. And doctors rarely ask about them.Why? Because they’re sold over the counter. No prescription means no warning. No pharmacist counseling. No flag in the electronic health record. But the science is clear: daily use of diphenhydramine for more than three years increases dementia risk by 54%, according to a 2015 JAMA Internal Medicine study of over 3,400 people. Antihistamines made up nearly a third of the strong anticholinergic drugs in that study.
It’s not just memory. People report dry mouth, blurry vision, trouble urinating, constipation, and dizziness. But the biggest red flag? Sudden confusion. Caregivers on Reddit describe relatives who were misdiagnosed with dementia-until someone noticed they were taking Benadryl every night, plus amitriptyline. Once both were stopped, their clarity returned within weeks.
How Medications Stack Up: The Dangerous Combinations
You don’t need five drugs to hit a dangerous score. Three common ones can do it:- Diphenhydramine (Benadryl) - ACB score 3
- Amitriptyline (for pain or depression) - ACB score 3
- Oxybutynin (for bladder control) - ACB score 3
That’s a total of 9. That’s not a mistake. That’s a crisis.
Even milder combinations add up fast:
- Chlorpheniramine (allergy) - ACB 2
- Hydroxyzine (anxiety or itching) - ACB 2
- Meclizine (motion sickness) - ACB 2
That’s 6. Still dangerous. And these are just the ones people know about. Many heartburn meds, Parkinson’s drugs, and even some muscle relaxants have hidden anticholinergic effects. One study found 40% of anticholinergic burden comes from drugs no one thinks of as brain-affecting.
What Does the Science Say About Long-Term Use?
The 2015 JAMA study wasn’t a fluke. It followed people for seven years. The longer someone took strong anticholinergics, the worse their memory got. People using them daily for over 1,095 days (three years) had a 54% higher risk of dementia than those who never took them. The risk didn’t go away after stopping-it was tied to how long they’d been exposed.And it’s not just dementia. A 2016 study from the IU Center for Aging Research showed people with high anticholinergic burden were 33% more likely to be hospitalized each year. Falls increased. Confusion spiked. Emergency visits went up. When researchers helped patients stop these drugs, hospital use dropped by up to 33% in a year.
The American Geriatrics Society updated its Beers Criteria in 2023 to say this plainly: “Chronic use of first-generation antihistamines should be avoided in older adults due to strong evidence of cognitive impairment even at low cumulative doses.” That’s not a suggestion. It’s a warning from the top medical experts in geriatrics.
Second-Generation Antihistamines Are the Safe Alternative
Here’s the good news: you don’t have to give up allergy relief. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) have an ACB score of 0 or 1. They don’t cross the blood-brain barrier like diphenhydramine does. They don’t cause drowsiness or memory fog.Switching isn’t hard. A 2021 NPS MedicineWise case study showed a 72-year-old woman with an ACB score of 5 (from diphenhydramine, oxybutynin, and amitriptyline) regained her balance, stopped falling, and remembered names within six months after switching to cetirizine and stopping the sedating drugs. Her family didn’t even notice the change until she started cooking again.
And the market is shifting. By 2022, 85% of new allergy prescriptions were for second-generation drugs. But among older adults, 40% still use the old ones-because they’re cheaper, familiar, or sold next to the candy aisle.
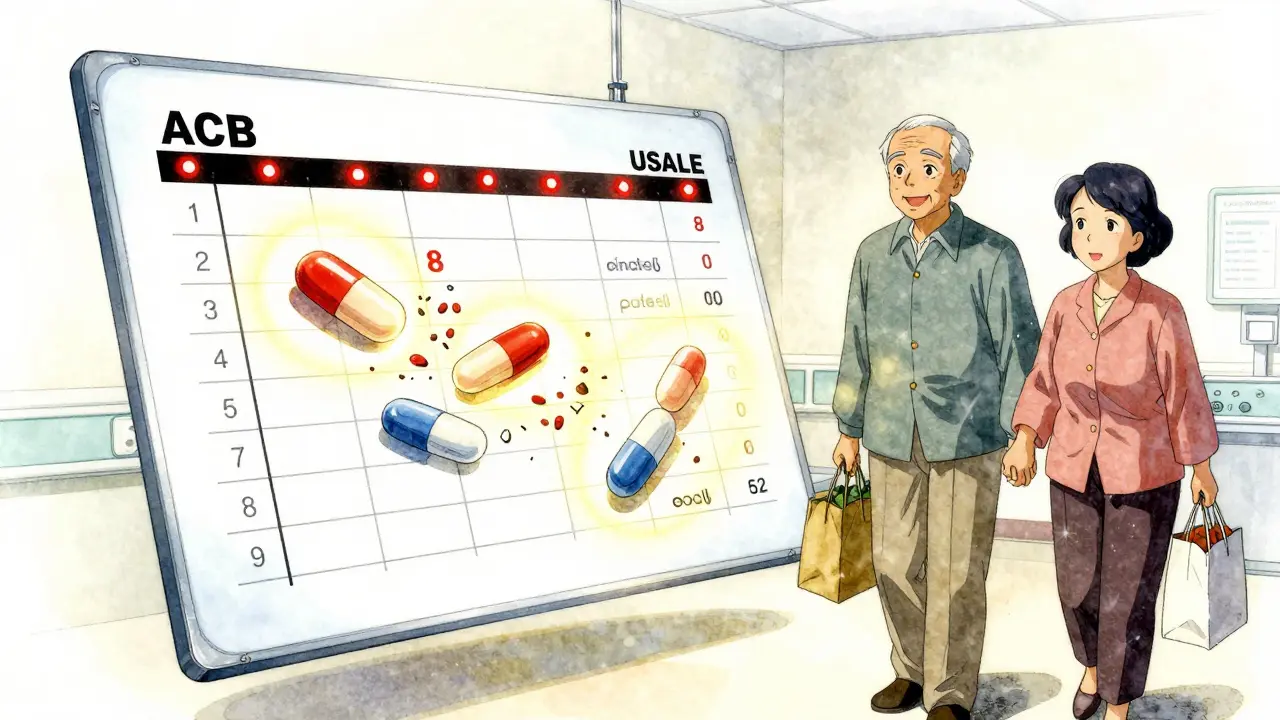
How to Check Your Own Burden
You don’t need a doctor to start. Here’s what to do:- Write down every pill, patch, or liquid you take daily-even vitamins and supplements.
- Look up each one on the ACB Scale (search “ACB Scale drug list” or check NPS MedicineWise resources).
- Add up the scores. If it’s 3 or higher, you’re in the danger zone.
- Ask your pharmacist: “Are any of these drugs anticholinergic?” Most pharmacists now know the scale.
- Ask your doctor: “Can we replace any of these with a non-anticholinergic option?”
Don’t stop anything cold turkey. But do start the conversation. Many people feel guilty asking to stop a “simple” pill. But if that pill is making you forget where you put your keys-or worse, making you fall-then it’s not simple anymore.
What Works: Real Cases of Recovery
A 78-year-old man in Perth was brought to the hospital after three falls in one month. His family thought it was aging. His doctor blamed his balance. But his medication list included diphenhydramine for sleep, amitriptyline for nerve pain, and oxybutynin for urinary urgency. ACB score: 8.They replaced diphenhydramine with melatonin. Switched amitriptyline to duloxetine (non-anticholinergic). Used a different bladder drug, solifenacin, with lower anticholinergic effect. Six weeks later, he hadn’t fallen again. His wife said he started remembering birthdays again.
This isn’t rare. The IU Center for Aging Research found that 65% of patients who were guided through a tapering plan successfully switched to safer alternatives within 4 to 8 weeks. The key? Support. A pharmacist review. A doctor who listens.
What’s Changing in 2026
Hospitals and clinics are waking up. In the U.S., Medicare plans now get better ratings if they reduce anticholinergic prescribing. Electronic health records are starting to flag high ACB scores automatically. The FDA and European Medicines Agency have added warnings to labels. But the biggest change? Awareness.By 2027, 80% of healthcare systems plan to screen patients over 65 for anticholinergic burden. That means your next appointment might include a quick checklist: “Are you taking any nighttime sleep aids or allergy pills?”
The goal isn’t to scare you. It’s to empower you. You don’t need to live with brain fog because you thought a pill was harmless. The science is clear. The alternatives exist. And the fix is often simple: swap the old for the new.
Can antihistamines really cause dementia?
Yes, long-term use of first-generation antihistamines like diphenhydramine and chlorpheniramine is linked to a higher risk of dementia. A 2015 JAMA study found people who used strong anticholinergics for more than three years had a 54% higher risk. The effect builds over time, even at low daily doses. Second-generation antihistamines like loratadine and cetirizine do not carry this risk.
What’s the difference between first and second-generation antihistamines?
First-generation antihistamines like Benadryl cross into the brain and block acetylcholine, causing drowsiness, memory issues, and dry mouth. Second-generation ones like Claritin and Zyrtec stay mostly outside the brain. They treat allergies without affecting cognition. They’re just as effective for sneezing and itching, but far safer for long-term use.
How do I know if my medication has anticholinergic effects?
Check the ACB Scale. Search online for “ACB Scale drug list” or ask your pharmacist. Common ones include diphenhydramine, chlorpheniramine, amitriptyline, oxybutynin, and meclizine. If you’re taking any of these regularly, especially with other meds, your burden may be too high. Don’t guess-look it up.
Is it safe to stop taking antihistamines cold turkey?
No. Stopping suddenly can cause rebound symptoms like severe itching or insomnia. Work with your doctor or pharmacist to taper off slowly. Replace them with non-anticholinergic options like cetirizine for allergies or melatonin for sleep. Most people transition safely within 4 to 8 weeks with a plan.
Can younger people get affected too?
The strongest evidence is in people over 65, but younger adults with multiple anticholinergic drugs can still experience drowsiness, confusion, or urinary issues. If you’re on three or more medications with anticholinergic effects, even under 65, it’s worth reviewing. The brain’s sensitivity to these drugs varies, but cumulative harm can start earlier than most think.


Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.