Every year, thousands of accidental poisonings happen in homes-not because someone meant to take the wrong pill, but because medications were stored carelessly. In Australia, as in many countries, the kitchen counter, bathroom cabinet, or bedside table might seem like convenient spots for pills, but they’re also the most dangerous. A medication storage checklist isn’t just a good idea-it’s a lifesaver. It stops kids from grabbing insulin like candy, prevents seniors from mixing up blood thinners, and keeps your drugs working as they should.
Why Your Medicine Cabinet Is the Worst Place to Store Pills
Most people think the bathroom cabinet is fine because it’s right next to the sink. But it’s actually one of the worst places in the house. Every time someone takes a hot shower, the humidity spikes to 80-90%. That moisture breaks down pills, creams, and inhalers faster than you think. Studies show that medications stored in bathrooms lose 30-50% of their potency within months. Heat from pipes and light from overhead bulbs make it worse. The same goes for the kitchen near the stove or a windowsill. Temperature swings, sunlight, and steam all degrade active ingredients. The FDA says even properly stored pills can lose up to 40% of their strength after 30 days of light exposure. If your aspirin or antibiotic isn’t working like it should, the problem might not be your body-it’s your storage.Where to Store Medications: The Ideal Spot
Forget the bathroom. Find a cool, dry, dark place that’s out of reach but easy for adults to access. A locked linen closet, a high drawer in a bedroom dresser, or a dedicated cabinet in a rarely used room works best. The goal is consistency: stable temperature (between 68-77°F) and low humidity (40-50%). If you have medications that need refrigeration-like insulin, some eye drops, or liquid antibiotics-they must stay between 36-46°F. Keep them in the main fridge, not the door, where temperatures bounce around. Put them on a shelf away from raw meat or dairy. Cross-contamination isn’t just a food issue-it’s a medication safety issue too.Organize by Person, Not by Type
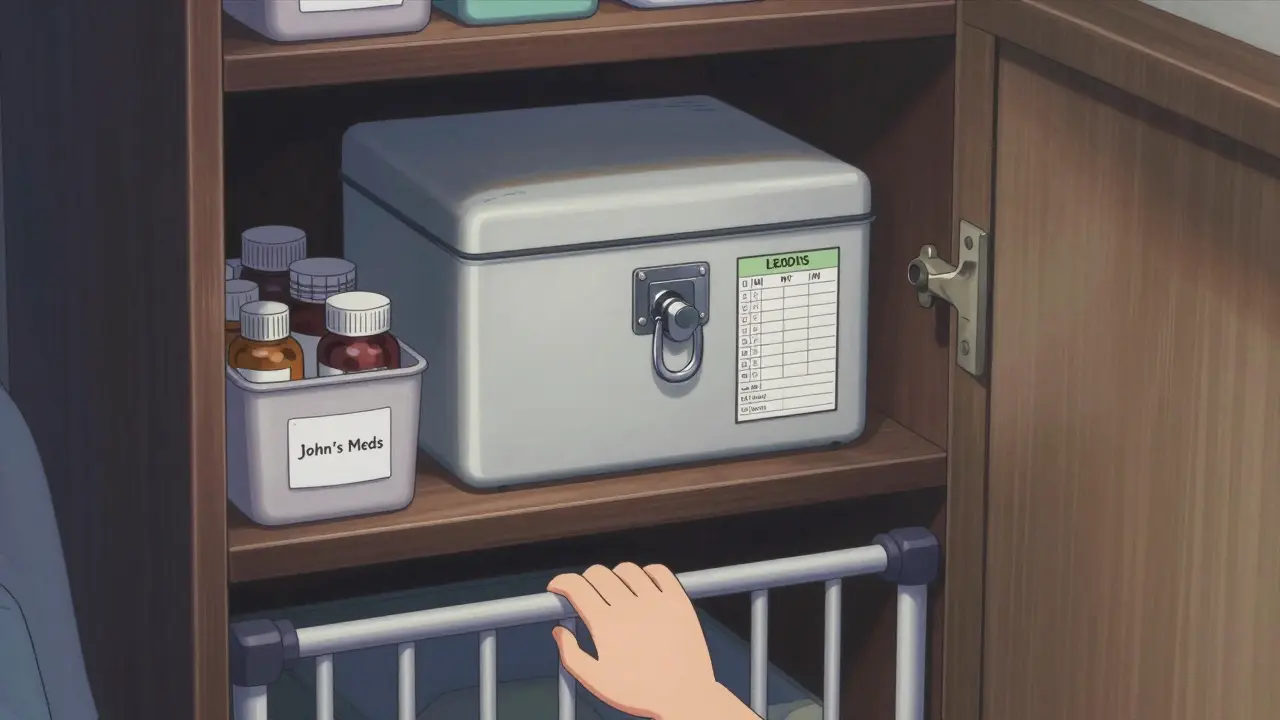
Mixing up medications is one of the biggest causes of accidental overdoses, especially in homes with multiple people. Grandma’s blood pressure pill looks nothing like Grandpa’s cholesterol pill-until you toss them all into one jar. That’s when mistakes happen. Your checklist should require each person’s meds to be stored separately. Use labeled bins, drawers, or boxes. If space is tight, divide one shelf with a divider and label each side clearly: “John’s Meds,” “Mary’s Meds.” A 2022 study found this simple step cut accidental wrong-medication use by 63%. For high-risk drugs-like opioids, insulin, or warfarin-go a step further. Use a small locked box inside your main storage area. Label it clearly: “High Alert.” This isn’t overkill. In Canada, homes using this method saw a 78% drop in medication errors.Lock It Down: Childproofing and Theft Prevention
A standard medicine cabinet? It’s useless against kids. The Consumer Product Safety Commission found that only 12% of children under 5 can’t open them. Even if the door has a latch, a determined 2-year-old with a spoon can pop it open in seconds. Use a dedicated medicine lockbox. These cost under $30 and come with combination locks or keypads. A 2023 Pediatrics study showed households using lockboxes had 92% fewer accidental ingestions by children under 5. Combination locks are 34% more reliable than key locks because no one forgets the code. Store meds at least 4 feet off the ground. Behind three closed doors? Even better. Most ingestions happen in places kids visit daily-bedrooms, living rooms, the kitchen. Make your storage spot unfamiliar to them. And never leave pills on a nightstand, even for “just a minute.” The American Academy of Pediatrics says 70% of childhood poisonings happen when meds are left unattended for less than 10 minutes.
Track Expiration Dates Like a Pro
Most people don’t know when their meds expire. The BeMedWise organization found that 70% of households keep at least one expired pill. That’s not just wasteful-it’s risky. The FDA says 82% of pills still work one year past their date if stored well. But at three years? Only 42% retain potency. Your checklist needs a clear expiration check schedule. Do it every six months-right after daylight saving time changes. That’s when most people are already thinking about home maintenance. Pull out every bottle. Check the printed expiration date. Look for signs of damage: pills that are cracked, discolored, or sticky. Creams that separate or smell odd. Inhalers with dents or leaking valves. For multi-dose items like insulin vials or eye drops, mark the date you opened them. Most lose effectiveness after 28-56 days, even if refrigerated. A 2022 study found that 38% of insulin users don’t track this-and their blood sugar control suffers as a result.Keep Everything in Original Packaging
Never transfer pills to pill organizers unless you’re using them for daily doses. Even then, keep the original bottle as your master copy. The label has the drug name, dosage, prescribing doctor, and pharmacy info. If something goes wrong-like a reaction or overdose-first responders need that info fast. This rule applies to everything: creams, nasal sprays, patches, even vitamins. North Carolina’s Kaitlyn’s Law requires this in childcare settings-and it reduced errors by 72%. Same logic applies at home. A bottle labeled “Lorazepam 1mg” is clear. A pill in a random container? That’s a hazard.Dispose of Expired or Unused Meds the Right Way
Don’t flush them. Don’t toss them in the trash unopened. Don’t dump them in the compost. Flushing sends pharmaceuticals into waterways-80% of U.S. streams now contain traces of drugs. Throwing them in the bin? That’s how pets and kids get into them. The safest method: use a drug take-back program. In Australia, pharmacies and police stations often host collection bins. The DEA’s National Prescription Drug Take Back Day collects over a million pounds of meds each year. Check your local council website for drop-off locations. If no take-back is available, mix pills with something unappetizing-used coffee grounds, kitty litter, or dirt-in a sealed container. The FDA says this reduces accidental ingestion by 76%. Then toss the container in the trash. Remove or black out your name on the label first.
Build Your Checklist: The 7-Point System
Here’s your simple, actionable checklist. Print it. Tape it to the inside of your medicine storage cabinet. Check it every six months.- 1. Location: Stored in a cool, dry, dark place-not bathroom, kitchen, or windowsill.
- 2. Temperature: Refrigerated items kept at 36-46°F; room temp meds between 68-77°F.
- 3. Separation: Each person’s meds stored separately, labeled clearly.
- 4. Security: All meds locked in a childproof box or cabinet, 4+ feet off ground.
- 5. Expiration: All bottles checked every 6 months; opened multi-dose items marked with date opened.
- 6. Packaging: All meds in original containers with labels intact.
- 7. Disposal: Expired or unused meds taken to a drop-off site or mixed with coffee grounds before trash disposal.
What to Do If You Find a Problem
If you spot a discolored pill, a leaking inhaler, or a bottle with no label, don’t guess. Call your pharmacist. They’ll tell you if it’s safe to use or if you need a replacement. Many pharmacies will replace expired meds at no cost if you bring them in. If you think someone has taken the wrong pill-even if they seem fine-call Poison Control immediately. In Australia, that’s 13 11 26. Don’t wait for symptoms. Time matters.Final Thought: This Isn’t Just About Pills
Your medication storage system isn’t just about safety-it’s about peace of mind. It means you won’t panic when your grandchild visits. It means your aging parent won’t accidentally double-dose. It means your asthma inhaler will work when you need it most. Start small. Pick one item on the checklist today. Lock the insulin. Move the painkillers. Check the expiration date on your antihistamines. Do one thing. Then do another next week. In six months, you’ll have a system that protects everyone in your home.Can I store all my medications in one container?
No. Storing different people’s medications in one container increases the risk of accidental ingestion or dosage errors. Even if the pills look similar, their effects and dosages can be dangerously different. Always keep each person’s meds in separate, labeled containers.
Is it safe to keep medications in the fridge?
Only if the label says so. Insulin, some antibiotics, and eye drops require refrigeration between 36-46°F. Store them on a shelf inside the fridge, not in the door. Keep them away from food and never store them with raw meat or fish to avoid contamination.
What should I do with old or expired medications?
Use a drug take-back program at a pharmacy or police station. If that’s not available, mix pills with used coffee grounds or kitty litter in a sealed container, then throw them in the trash. Remove or black out your personal info on the bottle first. Never flush them down the toilet.
How often should I check my medication storage?
Check your entire collection every six months-ideally when daylight saving time changes. Look for expired dates, damaged packaging, and changes in color or texture. Refrigerated meds need daily temperature checks, and opened multi-dose items should be labeled with the date opened.
Are over-the-counter drugs included in a medication storage checklist?
Yes. OTC drugs like pain relievers, allergy pills, and topical creams are just as dangerous if misused. Kaitlyn’s Law in North Carolina includes OTC products in its storage rules, and for good reason-children and seniors can accidentally overdose on them too.
What if I have a visitor who needs their medication?
Have them keep their meds in their own travel case or bag. Don’t add them to your home storage unless they’re staying long-term. If they do need to leave meds with you, label them clearly with their name and store them separately. Never mix visitor meds with yours.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.