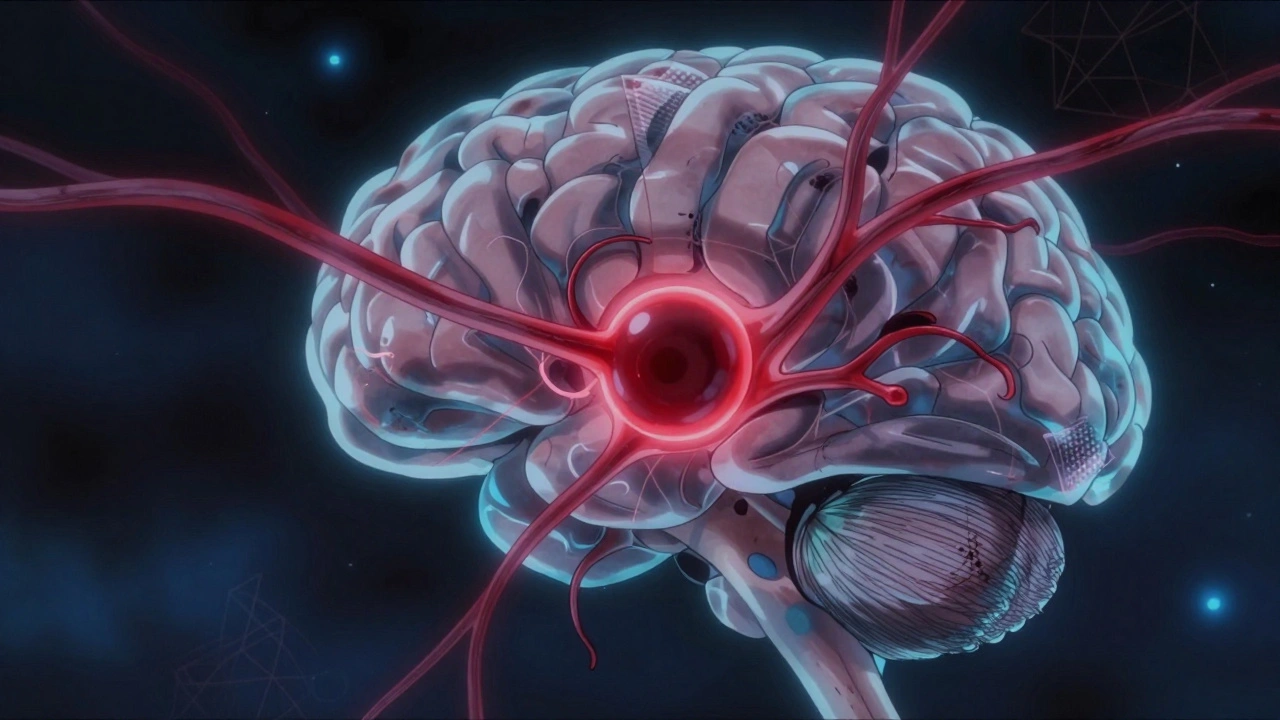
A cerebral aneurysm isn’t something you hear about until it’s too late. Most people never know they have one-until it bursts. Every year, about 10 in every 100,000 people experience a ruptured brain aneurysm. Half of them don’t make it past the first day. For those who survive, recovery is long, uncertain, and often life-changing. The good news? Many aneurysms never rupture. And when they do, we now have better ways to stop them before it’s too late.
What Exactly Is a Cerebral Aneurysm?
A cerebral aneurysm is a weak spot in the wall of a brain artery that balloons out like a tiny blister. It’s not a tumor. It’s not cancer. It’s a structural flaw in the blood vessel itself. Think of it like a bulge in an old garden hose-over time, pressure from blood flow stretches the wall thin. If it bursts, blood floods into the space around the brain, causing a subarachnoid hemorrhage. That’s a medical emergency.
These aneurysms form slowly, often over decades. They’re found in about 3.2% of adults worldwide, mostly during scans for other reasons. Most stay harmless. But some don’t. The risk isn’t random. It’s shaped by your body, your habits, and even your genes.
Who’s at Risk for Rupture?
Not all aneurysms are created equal. Some are ticking time bombs. Others are quiet, harmless bumps. The key is knowing what makes one more likely to burst.
Age matters. After 65, your risk jumps 2.7 times. The walls of your arteries naturally weaken over time. That’s why most ruptures happen in people over 50.
Gender plays a role. Women are 1.6 times more likely to develop aneurysms than men. Hormones, especially after menopause, may contribute to weaker vessel walls.
Family history is a red flag. If two or more close relatives had an aneurysm, your risk triples. It’s not just coincidence-it’s genetics. Certain inherited conditions like polycystic kidney disease or Ehlers-Danlos syndrome also raise the odds.
But here’s the part you can control:
- High blood pressure is the biggest modifiable risk. If your systolic pressure stays above 140, your rupture risk jumps by 2.3 times. Keeping it under 130/80 cuts that risk dramatically.
- Smoking is even worse. Current smokers face a 3.1 times higher risk. And it’s not just smoking-it’s how much. People who smoke 10 or more cigarettes a day see their risk climb by 47%.
- Heavy drinking (more than 14 drinks a week) increases rupture risk by 32%. Alcohol raises blood pressure and weakens vessel walls over time.
One study showed that quitting smoking reduces rupture risk by 54% within just two years. That’s not a small win. It’s a game-changer.
Shape, Size, and Location: The Silent Predictors
Doctors don’t just look at whether you have an aneurysm. They study its shape, size, and where it’s sitting in your brain.
Size is critical. An aneurysm smaller than 7 mm has a low rupture rate-often less than 1% per year. But once it hits 7 mm or larger, the risk jumps to 3.1 times higher. Giant aneurysms (over 25 mm) are almost always dangerous.
Shape tells the story. A smooth, round bulge is less risky. But if it has an irregular shape-like a lobe or a daughter sac sticking out-the risk doubles. These irregularities create turbulence in blood flow, which tears at the wall.
Location changes everything. Some spots are more dangerous than others. Aneurysms at the anterior communicating artery (AComm) are especially risky-even if they’re small. They rupture more often than others. Middle cerebral artery aneurysms also carry high risk. Meanwhile, aneurysms in the posterior circulation (back of the brain) are harder to treat and more likely to cause serious damage if they burst.
There’s even a rare but deadly pattern: aneurysms under 5 mm in the distal anterior cerebral artery can still rupture. That’s why size alone isn’t enough.
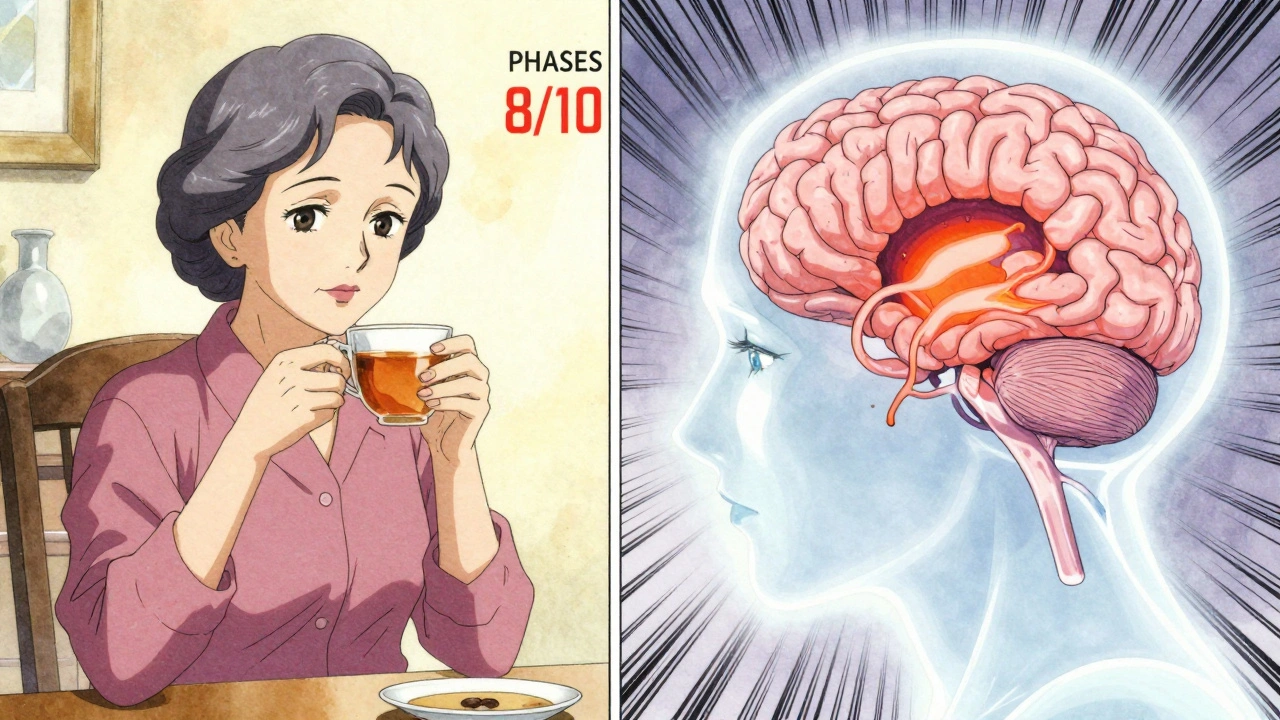
The PHASES Score: Your Personalized Risk Calculator
Doctors don’t guess. They use tools. The most trusted one is the PHASES score. It’s based on six factors:
- Population (where you live-some regions have higher rates)
- Hypertension (your blood pressure)
- Age (younger or older)
- Size of the aneurysm
- Earlier subarachnoid hemorrhage (if you’ve had one before)
- Site (location in the brain)
Each factor adds points. A score of 0-3 means your 5-year rupture risk is only 3%. A score of 9-10? That’s 45%. That’s not a small difference. That’s the difference between watching and acting.
Most guidelines say: if your PHASES score is 6 or higher, treatment should be considered. Below that? Monitoring might be safer than surgery.
Treatment Options: Clipping, Coiling, and Flow Diversion
If your aneurysm is high-risk, you have three main choices: surgical clipping, endovascular coiling, or flow diversion. Each has pros and cons.
Surgical Clipping
This is the original method, first done in 1937. A neurosurgeon opens your skull (craniotomy), finds the aneurysm, and places a tiny titanium clip across its neck. This stops blood from flowing into it.
It’s highly effective: 95% of clipped aneurysms are completely sealed. The cure is permanent. But it’s invasive. Recovery takes weeks. The risk of permanent brain injury is about 4.7%, and death occurs in 1.5% of cases.
Clipping works best for wide-necked aneurysms or those in hard-to-reach spots. But if you’re over 70, your complication risk rises by 35%.
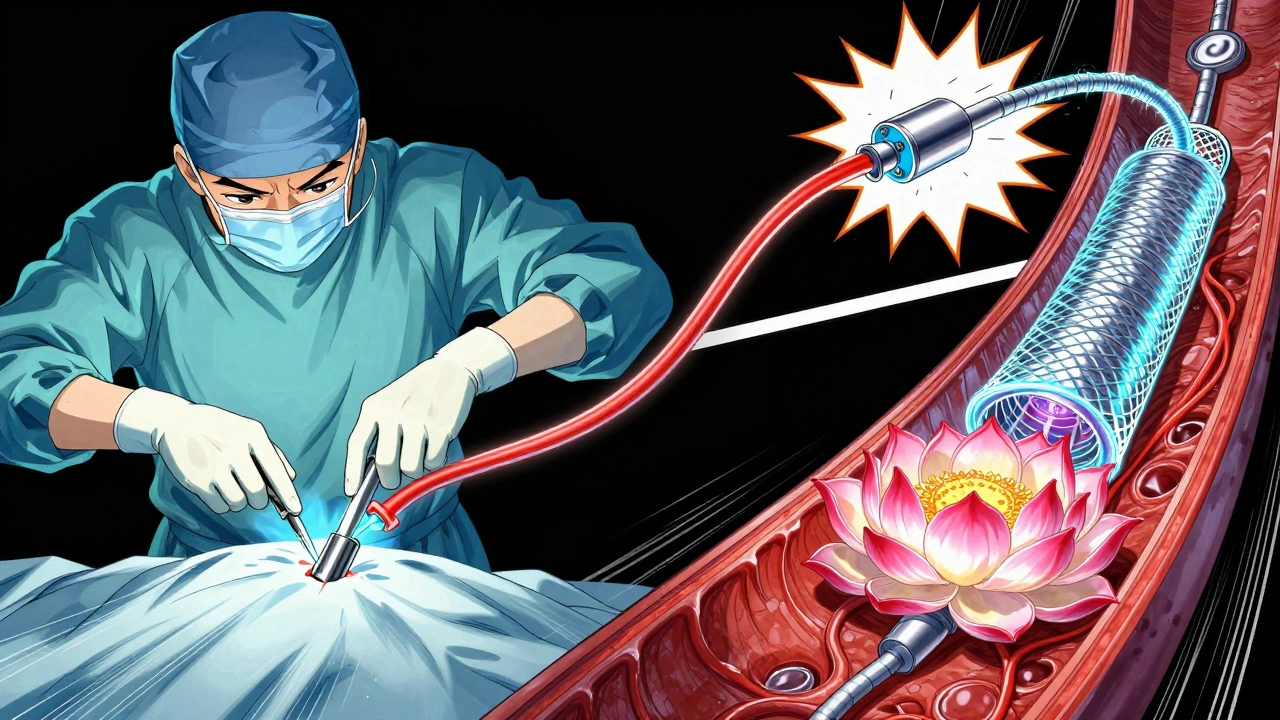
Endovascular Coiling
This is the less invasive option. A catheter is threaded from your groin up to your brain. Tiny platinum coils are pushed into the aneurysm. They trigger a blood clot inside it, sealing it off.
Success rates? Around 78-85% at six months. It’s faster to recover from. Most people go home in a day or two. But there’s a catch: 15-20% of coiled aneurysms slowly reopen over time. You’ll need regular scans for years.
Coiling is preferred for older patients, those with health issues, and aneurysms in the front of the brain. It cuts 1-year mortality by 22% compared to clipping.
Flow Diversion
This is the newest approach. Instead of filling the aneurysm, you redirect blood flow away from it using a special mesh stent-like a tiny net placed across the artery. Blood flows through the stent, not into the aneurysm. Over time, the aneurysm shrinks and disappears.
It’s ideal for large, wide-necked, or complex aneurysms that can’t be treated with coils alone. The Pipeline Embolization Device and WEB device are FDA-approved. One-year occlusion rates hit 85% with newer models.
But it’s not perfect. You need to take blood thinners for months. And there’s a small risk of stroke during healing. Morbidity is around 5.2%, slightly higher than coiling.
What About Watching and Waiting?
Not every aneurysm needs treatment. In fact, most don’t.
The UCAS Japan study showed that small aneurysms under 5 mm in the anterior circulation have only a 0.2% chance of rupturing over five years. That’s lower than the risk of a car accident on your daily commute.
If your aneurysm is small, round, in a low-risk location, and your PHASES score is below 6, doctors often recommend monitoring. That means:
- Annual MRA scans to check for growth
- Strict blood pressure control
- Quitting smoking
- Avoiding heavy alcohol
Some patients go years-sometimes decades-without any intervention. The goal isn’t to panic. It’s to stay informed and proactive.
What Happens After Treatment?
Success isn’t just about sealing the aneurysm. It’s about living well afterward.
Successful treatment drops your 10-year re-rupture risk from 68% to just 2.3%. That’s huge.
Quality of life matters too. People who get coiling or flow diversion report better scores on quality-of-life measures (EQ-5D) than those who have surgery. They return to work faster, feel less pain, and have fewer long-term limitations.
But recovery isn’t instant. Brain healing takes time. Some people deal with fatigue, memory issues, or mood changes for months. That’s normal. Support groups, rehab, and patience help.
The Future: Genetics and AI
We’re entering a new era. Researchers are now looking at your genes to predict risk. The HUNT study found 17 genetic markers linked to aneurysm formation and rupture. In the future, a simple blood test might tell you if you’re at high genetic risk-even before an aneurysm forms.
Artificial intelligence is also stepping in. Machine learning models now analyze hundreds of data points-aneurysm shape, blood flow patterns, wall thickness-to predict rupture better than any scorecard. One model had a 72% accuracy rate (C-index of 0.72). That’s better than doctors relying on size alone.
These tools won’t replace doctors. But they’ll help them make smarter, faster decisions.
What Should You Do Now?
If you’ve been told you have a cerebral aneurysm, don’t panic. But don’t ignore it either.
Ask your doctor:
- What’s my PHASES score?
- What’s the size, shape, and location?
- Do I have a family history?
- Am I a smoker or have high blood pressure?
- What are my treatment options-and what are the risks of each?
- Can I wait and monitor, or should I act now?
And if you haven’t been diagnosed but you’re over 50, have high blood pressure, smoke, or have a family history-talk to your doctor about screening. A simple MRA or CTA scan can detect an aneurysm before it’s a crisis.
Brain aneurysms aren’t always a death sentence. With the right information, the right care, and the right choices, many people live full, healthy lives-even with one.
Can a cerebral aneurysm go away on its own?
No, a cerebral aneurysm won’t disappear without treatment. But in rare cases, a small aneurysm may clot off naturally due to slow blood flow. This is unpredictable and not something to rely on. Medical monitoring is essential-never assume it’s gone just because you feel fine.
Is a brain aneurysm hereditary?
Yes, if two or more close relatives (parents, siblings, children) had a ruptured or unruptured brain aneurysm, your risk increases fourfold. Certain genetic disorders like polycystic kidney disease or connective tissue conditions also raise the risk. If you have a family history, screening is strongly recommended after age 25.
Can stress cause a brain aneurysm to rupture?
Extreme stress-like intense physical exertion, sudden anger, or a major emotional shock-can spike blood pressure and trigger rupture in a vulnerable aneurysm. But chronic stress alone doesn’t cause aneurysms. The real danger is uncontrolled high blood pressure, which is often worsened by stress. Managing stress helps, but controlling blood pressure is the key.
Do all brain aneurysms need surgery?
No. Many small, stable aneurysms-especially under 7 mm and in low-risk locations-can be safely monitored. Treatment is recommended when the risk of rupture outweighs the risk of treatment. This depends on size, shape, location, your age, and overall health. About 70% of unruptured aneurysms are managed without surgery.
How often should I get scanned if my aneurysm is being monitored?
For small, stable aneurysms, annual MRA scans are standard. If the aneurysm grows or changes shape, scans may be done every 6 months. If there’s no change after 2-3 years, your doctor may extend the interval. Never skip scans-even if you feel fine. Growth is often silent.
Can I exercise with an unruptured brain aneurysm?
Yes, but with caution. Light to moderate exercise like walking, swimming, or cycling is safe and encouraged. Avoid heavy weightlifting, intense isometric exercises, or activities that cause sudden spikes in blood pressure (like competitive sports or CrossFit). Always check with your neurologist before starting a new routine.
What are the signs of a ruptured brain aneurysm?
A ruptured aneurysm causes a sudden, severe headache-often described as the worst headache of your life. Other signs include nausea, vomiting, stiff neck, blurred vision, sensitivity to light, seizures, or loss of consciousness. If you or someone else has these symptoms, call emergency services immediately. Every minute counts.
Are there any natural remedies or supplements that help?
No supplement or herb can shrink or prevent rupture of a brain aneurysm. Some, like ginkgo biloba or fish oil, may thin the blood and increase bleeding risk. Don’t take anything without talking to your doctor. The only proven natural interventions are quitting smoking, lowering blood pressure, and reducing alcohol intake.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.