Every year, over 23,000 people in the U.S. end up in the emergency room because of dangerous mix-ups between their supplements and medications. That’s not a small number - it’s more than double what it was in 2010. And here’s the scary part: most of these people had no idea their daily vitamin or herbal pill could be making their heart medicine, antidepressant, or blood thinner less effective - or even toxic.
You’re not alone if you take supplements. About 75% of American adults use them. But only about 32% of people over 50 - the group most likely to be on multiple medications - ever tell their doctor about it. That gap is deadly. A supplement labeled "natural" doesn’t mean it’s harmless. In fact, some of the most dangerous interactions come from things you can buy off a shelf at your local pharmacy or grocery store.
What Makes a Supplement Dangerous with Medications?
It’s not magic. It’s chemistry. Your body uses enzymes - mostly in the liver - to break down drugs. One group, called cytochrome P450, handles about 60% of all prescription medications. Some supplements mess with these enzymes like a wrench thrown into a gearbox.
St. John’s wort is the worst offender. It forces your body to break down drugs too fast. That means your birth control pill stops working. Your transplant drug (like cyclosporine) drops by half its effectiveness. Your antidepressant might not help at all. Studies show it can reduce blood levels of over 57 different medications by 30% to 60%. And it’s not rare - Drugs.com has over 1,200 user reports of problems with it.
Then there’s the opposite problem: supplements that slow down drug breakdown. Ginkgo biloba, for example, doesn’t interfere with most drugs - unless you’re on warfarin. Then it can double your risk of bleeding. Vitamin E at 400 IU or more does the same thing. Both make your INR (a blood clotting test) spike, which can lead to internal bleeding, stroke, or worse.
Minerals like calcium, magnesium, zinc, and iron compete for the same absorption spots in your gut. If you take iron for anemia and a calcium supplement for bone health at the same time, your body absorbs less of both. That means your iron pills stop working, and your bones still weaken.
Which Supplements Are Most Risky?
Not all supplements are created equal when it comes to drug interactions. Some are mostly safe. Others are ticking time bombs.
High-risk (avoid with most prescriptions):
- St. John’s wort - interacts with 57+ drugs including antidepressants, birth control, blood thinners, and transplant meds.
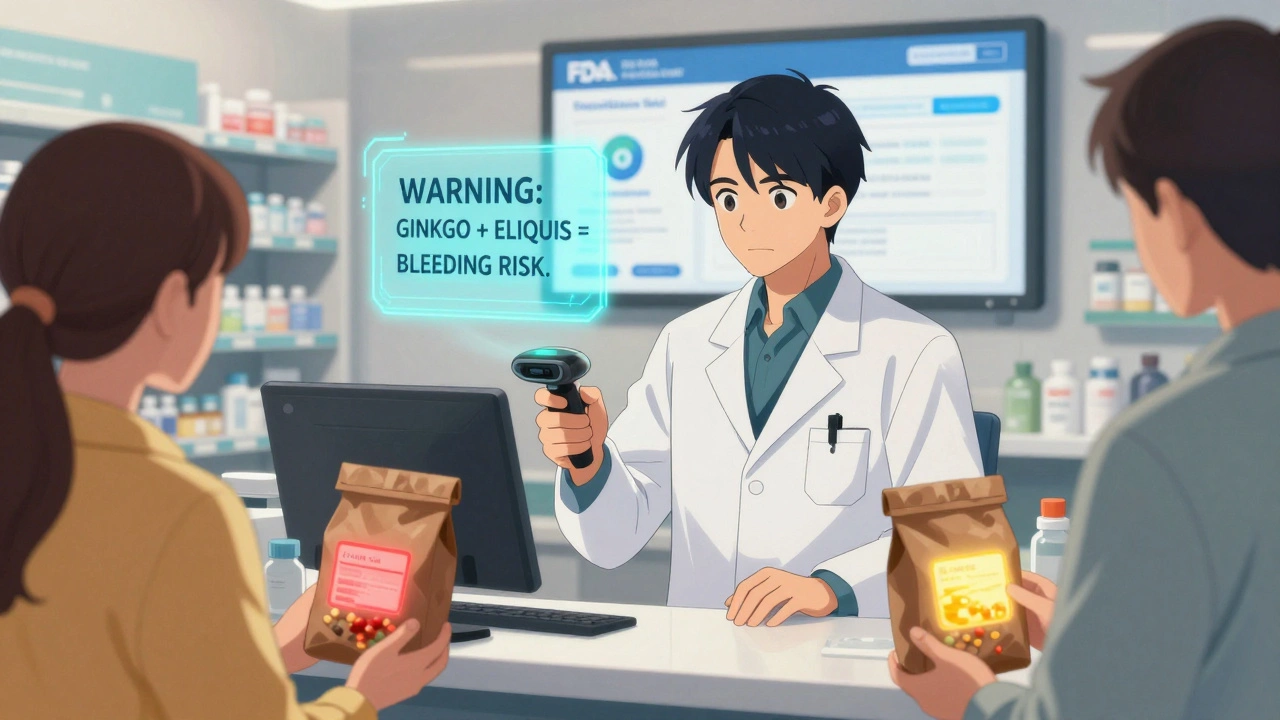
- Ginkgo biloba - safe for most, but deadly with warfarin, aspirin, or Eliquis. Can cause serious bleeding.
- Vitamin E (400 IU+) - increases bleeding risk when taken with blood thinners.
- Garlic, ginger, fish oil - all thin the blood. Surgeons ask you to stop these 7-10 days before surgery.
- Goldenseal - blocks liver enzymes and can raise levels of drugs like cyclosporine and statins to toxic levels.
Lower-risk (usually safe, but still check):
- Milk thistle - only 3 documented interactions in the last 10 years.
- Black cohosh, cranberry, American ginseng - very few proven interactions.
- Valerian, saw palmetto - generally safe, but avoid before surgery.
Even "safe" supplements can become risky if you’re on a drug with a narrow therapeutic index - meaning the difference between a helpful dose and a toxic one is tiny. That includes warfarin, digoxin, cyclosporine, and thyroid meds. If you take any of these, treat every supplement like a potential hazard.
Real Stories: When Supplements Go Wrong
A Reddit user named "PharmaTech87" took ginkgo biloba for memory and Eliquis for atrial fibrillation. He didn’t think twice about it - both were "natural." Within weeks, he started vomiting blood. He spent seven days in the hospital. His doctors said the combination caused a major GI bleed. He’s lucky he survived.
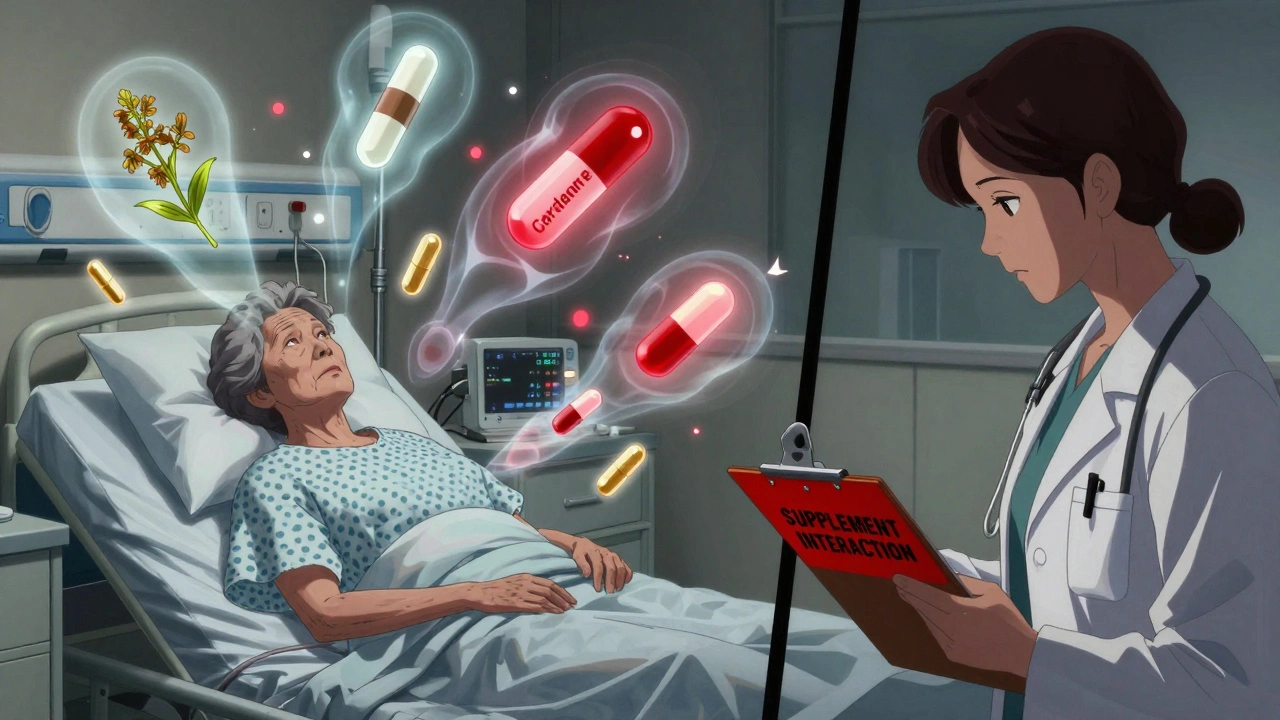
Another case: a 68-year-old woman in Ohio took St. John’s wort for depression while on her heart medication, Cordarone (amiodarone). Her doctor didn’t ask about supplements. She started feeling weak and dizzy. Her creatine kinase levels - a marker for muscle damage - shot up. She was diagnosed with rhabdomyolysis, a condition where muscle breaks down and floods the kidneys. Her simvastatin dose (a cholesterol drug) had been increased to 40 mg, and combined with Cordarone and St. John’s wort, her risk of muscle destruction went up 15-fold.
These aren’t outliers. They’re textbook examples of what happens when people assume supplements are harmless.
How to Check Your Own Supplements
You don’t need a PhD to protect yourself. Just follow these four steps:
- Make a complete list. Write down every pill, capsule, powder, tincture, or tea you take - including vitamins, herbs, probiotics, and even CBD. Don’t forget the ones you only take occasionally.
- Bring it to your appointment. The FDA calls this the "brown bag method." Take your bag of supplements to your doctor or pharmacist. They’ll check for conflicts you didn’t even know existed. A Johns Hopkins study found this cuts medication errors by 37%.
- Read the label. Look for "Warning" statements. If it says "Do not take with blood thinners" or "May interact with antidepressants," pay attention. The FDA now requires this on many labels - but not all. If it’s missing, assume the worst.
- Ask your pharmacist. Pharmacists are trained to spot interactions. Walgreens and CVS have mandatory screening programs. In 2021, they caught dangerous combinations in 18% of cases. That’s nearly one in five people.
And here’s a pro tip: take your supplements at least two hours apart from your medications. It won’t stop enzyme interactions, but it can help with absorption competition - especially for minerals like iron and calcium.
Why Doctors Don’t Always Ask - And What to Do
Most doctors don’t ask about supplements because they’re not trained to. A 2023 American Medical Association policy changed that - now physicians are required to screen for supplement use during every medication review. But not every clinic has caught up yet.
So don’t wait for them to ask. Say it first. "I’m taking St. John’s wort for my mood. Is that okay with my blood pressure pill?" Or: "I’ve been using fish oil for my joints. Should I stop before my surgery?"
And if your doctor says, "It’s fine," ask: "Is there any research showing it’s safe with my specific meds?" If they can’t point to a study, get a second opinion from a pharmacist.
What’s Changing in 2025?
The FDA is finally catching up. In late 2024, they’re launching a free mobile app called the Dietary Supplement Ingredient Database. You’ll be able to scan the barcode on your supplement bottle and instantly see if it interacts with any of your medications. It’s based on data from the National Institutes of Health and will include over 80,000 products.
Hospitals are also starting to integrate supplement data into electronic health records. Epic Systems, which runs records for 15% of U.S. hospitals, now flags potential interactions automatically. If your doctor prescribes you a new drug, the system might pop up: "Warning: Patient takes St. John’s wort - may reduce effectiveness."
But until you’re in one of those systems, you’re still your own best defense.
Bottom Line: Don’t Guess. Check.
You wouldn’t mix bleach and ammonia. You wouldn’t take two painkillers at once without checking. So why treat supplements differently? They’re not candy. They’re active chemicals - and they react with your medications in ways you can’t predict.
There’s no shortcut. No "I’ve been taking it for years" excuse. Your body changes. Your meds change. Your supplements change. What was safe last year might be dangerous now.
Take the 10 minutes to make a list. Bring it to your next appointment. Ask your pharmacist. Use the new FDA app when it drops. You don’t need to stop your supplements. You just need to know if they’re safe - with your specific meds, your specific health, your specific life.
Because "natural" doesn’t mean safe. And your life isn’t worth gambling on.


Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.