PHQ-9 Tracker: Monitor Your Depression Symptoms
About PHQ-9
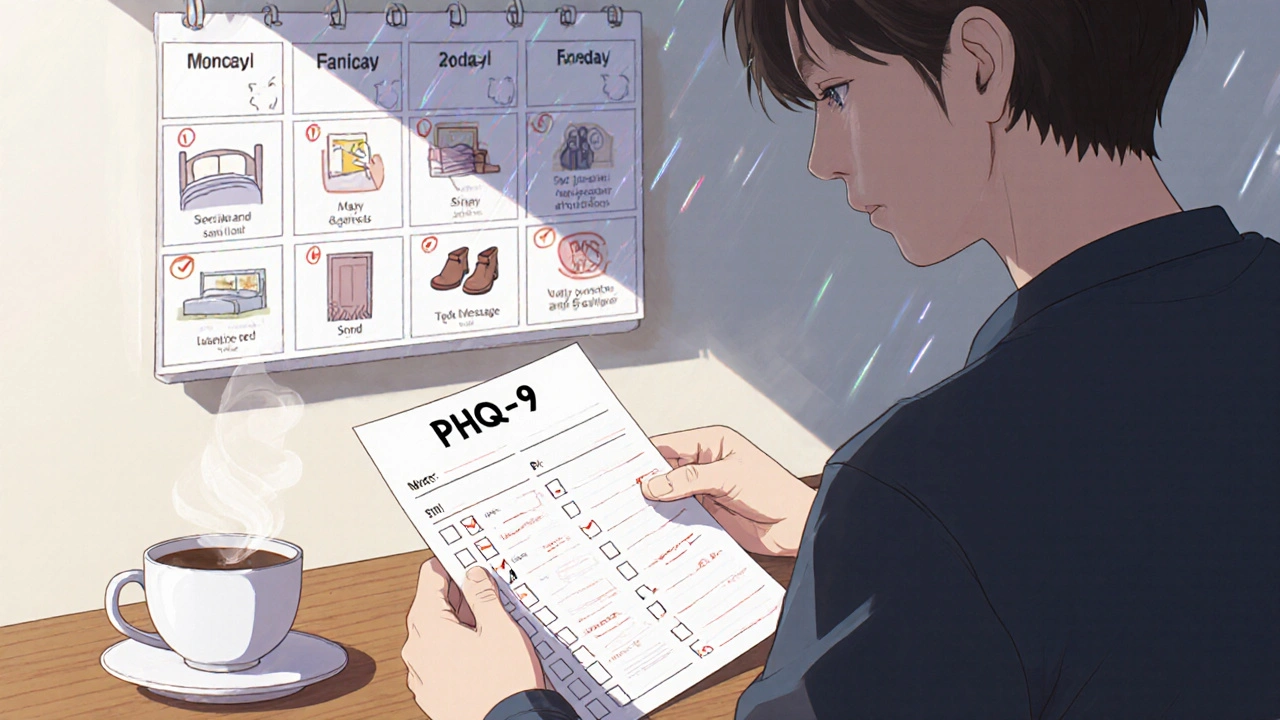
The PHQ-9 is a validated 9-question depression screening tool that measures how often you've felt down, lost interest, had trouble sleeping, or felt worthless over the past two weeks. Each question is scored 0-3 (not at all to nearly every day). Your total score helps your doctor understand your depression severity.
Track Your Symptoms
Your Results
Track Your Progress
Getting prescribed an antidepressant is only the first step. For many people, the real challenge begins after that first pill - figuring out whether it’s actually helping, and whether the side effects are worth it. You might feel a little better after a few weeks, but then you notice your sleep is wrecked, your libido vanished, or your hands won’t stop shaking. Or maybe you don’t feel anything at all. That’s not unusual. About 30-40% of people don’t get real relief from their first antidepressant, and 74% deal with at least one bothersome side effect. The key isn’t just taking the medicine - it’s knowing how to track what’s happening, so you and your doctor can make smart changes.
Why Tracking Matters More Than You Think
Most doctors don’t have magic tools to see if an antidepressant is working. They rely on what you tell them. But if you say, “I’m okay,” or “Better than before,” that’s not enough. Depression doesn’t vanish in one big moment. It fades slowly - sometimes in small ways you don’t even notice. Maybe you started making coffee again. Or you texted a friend back. Or you didn’t cry during your favorite TV show. Those are wins. But without tracking them, they get lost. The same goes for side effects. If you’re too tired to talk about them, or you think they’re just “part of being depressed,” they’ll keep dragging you down. That’s why structured monitoring isn’t optional - it’s the difference between staying stuck and finally moving forward. Studies show that when patients and doctors track symptoms and side effects using simple tools, remission rates jump by 50-60% compared to just guessing.The Three Tools You Need to Start Tracking
You don’t need fancy machines or expensive tests. Three simple tools can give you real clarity.- PHQ-9: This is a 9-question form that asks how often you’ve felt down, lost interest, had trouble sleeping, or felt worthless over the past two weeks. Each answer is scored 0 to 3. Add them up. A score under 5 means you’re likely in remission. A score above 15 means your depression is still moderate to severe. Do this once a week - it takes less than five minutes.
- BDI (Beck Depression Inventory): A slightly longer version with 21 questions. It’s great if you want to dig deeper into how your thoughts and physical symptoms are changing. A score above 29 means severe depression. You can find free printable versions online.
- ASEC (Antidepressant Side-Effect Checklist): This lists 15 common side effects - dry mouth, nausea, weight gain, sexual problems, dizziness. Rate each from 0 (not at all) to 4 (severe). Keep this in your phone notes or a small notebook. Review it every two weeks.
These aren’t just paper tests. They’re conversation starters. Bring them to your appointments. If your doctor doesn’t ask for them, offer them. You’re not being difficult - you’re giving them the data they need to help you.
What to Look For: Signs It’s Working
Don’t wait for “happiness” to show up. Look for small, measurable changes:- Are you getting out of bed 30 minutes earlier than before?
- Have you eaten three meals in a row this week?
- Did you answer a text without overthinking it?
- Did you go for a walk without needing to force yourself?
By week 6, you should see at least a 50% drop in your PHQ-9 or BDI score. If you don’t, it’s time to talk about adjusting the dose or switching meds. Waiting longer than 8 weeks without progress means you’re likely not responding - and every extra week without help makes recovery harder.
Some people feel worse before they feel better. That’s normal in the first 1-2 weeks. But if your anxiety spikes, you feel suicidal, or you can’t sleep for days - call your doctor immediately. Don’t wait for your next appointment.
Side Effects You Can’t Ignore
Not all side effects are equal. Some are annoying. Others are dangerous.- Sexual dysfunction: This is the #1 reason people quit SSRIs. If your libido vanishes or you can’t reach orgasm, tell your doctor. It’s not something you have to live with. Options include lowering the dose, switching to bupropion (which rarely causes this), or adding a medication like bupropion or sildenafil - yes, the one for erectile dysfunction - under supervision.
- Weight gain: Common with mirtazapine and paroxetine. If you gain more than 5% of your body weight in 3 months, it’s time to reassess. Try switching to sertraline or escitalopram, which are less likely to cause this.
- Emotional blunting: Feeling numb instead of sad? You’re not alone. About 1 in 3 people on SSRIs report this. It’s not “just being calm.” It’s losing the ability to feel joy, grief, or even anger. If this happens, talk about switching to SNRIs like venlafaxine or duloxetine, which often preserve emotional range better.
- Heart rhythm changes: Rare, but serious. If you’re on a TCA like amitriptyline and have a history of heart problems, ask for an ECG before starting. TCAs can slow your heart’s electrical signals - and that’s dangerous if your levels get too high.
Don’t downplay side effects. If you’re having trouble breathing, your chest feels tight, or your heartbeat races for no reason - go to the ER. These aren’t “normal” side effects. They’re red flags.
How to Use Digital Tools Without Getting Fooled
Apps like Moodfit and Sanvello can help you log mood, sleep, and side effects. They’re convenient. But they’re not perfect. A 2021 study found they only match paper-based scales about 72% of the time. That means they’re good for noticing patterns - but not for making final decisions.Use them as a diary, not a doctor. If you notice you feel worse every time you skip breakfast, or your anxiety spikes after caffeine - that’s real data. Share it with your provider. But don’t let the app tell you to “increase your dose” or “switch meds.” Only a clinician can do that.
Some apps now integrate with PHQ-9 and BDI. Use those. They’re validated. Avoid apps that promise “instant healing” or “AI diagnoses.” They’re not FDA-cleared. The only digital tool cleared by the FDA for antidepressant monitoring is Rejoyn - and even that just reminds you to fill out your PHQ-9 each week.
When to Ask for Blood Tests (TDM)
Therapeutic Drug Monitoring (TDM) sounds complicated, but it’s just a blood test that measures how much of the drug is in your system. It’s not for everyone. But if you’ve been on the same dose for 6 weeks and feel nothing - or if you’re having weird side effects despite taking it as prescribed - ask for it.Here’s why it matters: 50-70% of people who don’t respond to antidepressants actually have drug levels too low to work - even though they’re taking the pills. Maybe they’re a fast metabolizer. Maybe they’re taking something that interferes with absorption. TDM finds out.
It’s not cheap - $50 to $150 per test - and most insurance won’t cover it unless you’ve tried at least two meds. But if you’re stuck, it’s worth it. Studies show TDM-guided treatment improves remission rates by 25-35%.
What Your Doctor Should Be Doing - But Often Isn’t
You shouldn’t have to fight to get monitored. Here’s what good care looks like:- Baseline PHQ-9 or BDI before starting any antidepressant.
- Follow-up scores every 2-4 weeks during the first 3 months.
- ASEC checklist at each visit to track side effects.
- Discussion of treatment goals - not just “feel better,” but “go back to work 3 days a week” or “play with my kids without crying.”
- Offering TDM if no improvement after 6-8 weeks.
But here’s the hard truth: In primary care, only 32% of doctors use these tools regularly. Even in psychiatry, it’s only 68%. That means most people are being treated on guesswork. Don’t be one of them. Bring your own tracking sheets. Ask, “Are we measuring my progress?” If they say no - ask why. If they don’t have an answer, consider finding someone who does.
Real Stories: What Works
One woman in Perth, on sertraline for 9 months, felt “fine but empty.” She started using PHQ-9 every Sunday. Her score dropped from 18 to 12 - but she still felt nothing. Then she noticed: her energy improved on days she walked 10,000 steps. She added daily walks. In 4 weeks, her score hit 6. She wasn’t “cured,” but she was living again. Another man on fluoxetine had terrible sexual side effects. He told his doctor, who switched him to bupropion. His PHQ-9 stayed stable, but his libido returned. He stopped feeling like a side effect statistic.These aren’t miracles. They’re results of tracking, speaking up, and refusing to accept “it’s just how it is.”
What to Do Next
Start today. Print the PHQ-9. Download a free mood tracker. Write down one side effect you’ve been ignoring. Bring it to your next appointment. Don’t wait for your doctor to ask. You’re the expert on how you feel. They’re the expert on what to do with that information.Antidepressants aren’t magic. They’re tools. And like any tool, they only work if you know how to use them - and when to ask for a better one.
How long should I wait before deciding if my antidepressant is working?
Most antidepressants take 4 to 8 weeks to show full effects. But you should see at least a 50% drop in your PHQ-9 or BDI score by week 6. If you don’t, talk to your doctor about adjusting the dose or switching meds. Waiting longer than 8 weeks without improvement means you’re likely not responding - and every extra week delays your recovery.
Can I stop taking my antidepressant if the side effects are too bad?
Never stop abruptly. Stopping suddenly can cause withdrawal symptoms like dizziness, nausea, brain zaps, or rebound anxiety. Instead, talk to your doctor. They can help you taper slowly - usually over 2 to 6 weeks - to avoid these issues. If side effects are unbearable, ask about switching to a different medication with a better side effect profile for you.
Is it normal to feel emotionally numb on antidepressants?
Yes, it’s common - especially with SSRIs. About 1 in 3 people report feeling emotionally flat, like they’ve lost the ability to feel joy, sadness, or anger. This isn’t just “being calm.” It’s emotional blunting. If this happens, tell your doctor. Switching to an SNRI like venlafaxine or adding bupropion can help restore emotional range without losing the benefits of the antidepressant.
Do I need a blood test to check if my antidepressant is working?
Not always, but it can be very helpful if you’re not responding. About half of people who don’t improve have drug levels too low - even if they’re taking their pills. A blood test called Therapeutic Drug Monitoring (TDM) measures how much of the drug is in your system. It’s not routine, but if you’ve tried two meds with no results, ask your doctor about it. Studies show TDM improves remission rates by 25-35%.
Can I use a mood-tracking app instead of paper scales?
Apps like Moodfit and Sanvello can help you track mood and side effects daily, which is great for spotting patterns. But they’re not as accurate as paper-based scales like PHQ-9 or BDI - their consistency is around 72%, compared to 85%+ for paper tools. Use apps as a diary, not a diagnostic tool. Always verify your app data with a validated scale at least once a week, and bring those numbers to your doctor.
What if my doctor won’t use tracking tools?
Many doctors still rely on vague questions like “How are you feeling?” That’s not enough. Bring printed PHQ-9 and ASEC forms to your appointment. Say: “I’ve been tracking my symptoms and side effects using these tools. Can we review them together?” If they refuse or dismiss you, consider finding a provider who uses Measurement-Based Care. Your recovery depends on data - not guesswork.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.