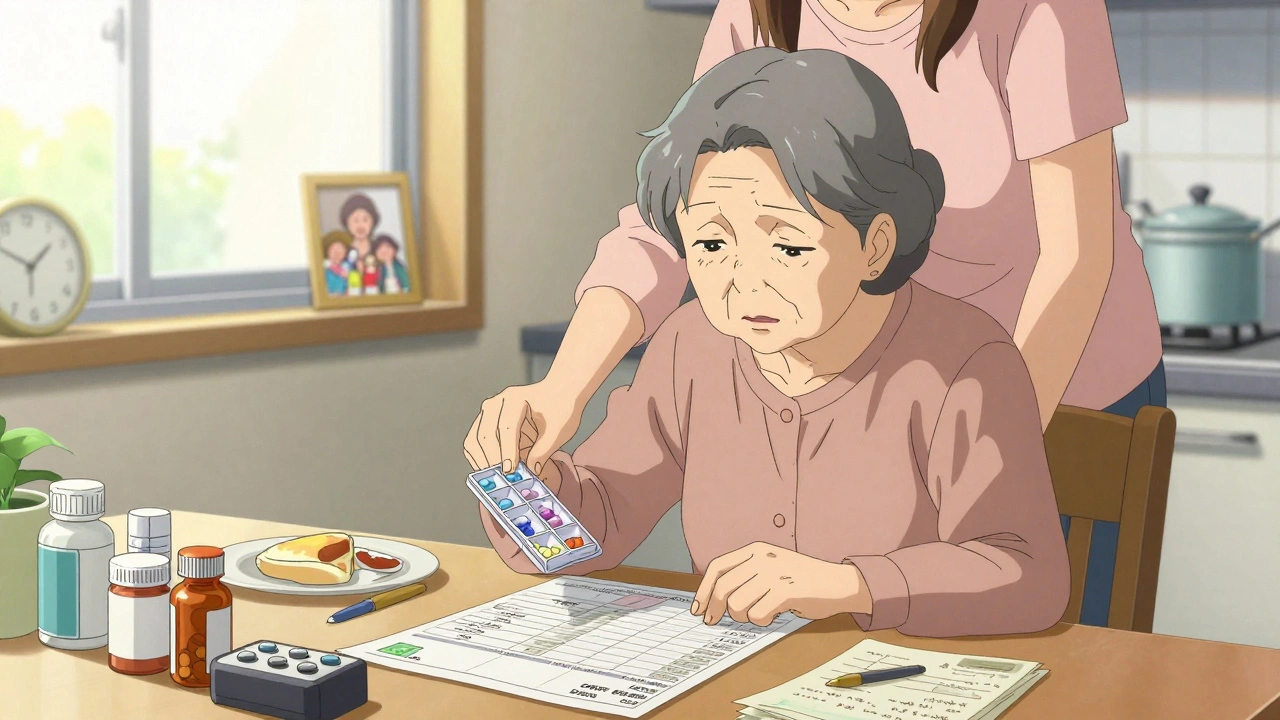
For many older adults, taking medications isn’t just a routine-it’s a full-time job. Picture this: a 78-year-old woman wakes up at 6 a.m. to take four pills, then again at 8 a.m. for three more, another two at noon, three in the afternoon, and two more before bed. That’s 14 doses a day, spread across seven different times. Many of these pills are for conditions like high blood pressure, diabetes, arthritis, or heart failure. But she’s forgetful. Some days, she skips a dose. Other days, she takes the wrong one. Her daughter, who lives an hour away, notices she’s not eating well and seems more confused. She’s not lazy. She’s overwhelmed.
This isn’t rare. In Australia, nearly 40% of adults over 65 take five or more medications daily. That number has tripled since the 1990s. And it’s not just about quantity-it’s about complexity. Different times, different forms (pills, liquids, patches), conflicting instructions ("take on an empty stomach," "avoid dairy"). The result? Poor adherence. Increased hospital visits. Falls. Confusion. And a growing sense of helplessness.
What Is Medication Regimen Simplification?
Medication regimen simplification means making it easier to take medicines without changing their purpose. It’s not about cutting drugs. It’s about cutting confusion. Think of it like streamlining your morning routine: instead of switching shoes, socks, and pants three times, you wear one outfit that works for everything. The same idea applies to pills.
There are three main ways this happens:
- Combining pills-switching from two separate tablets to one that contains both drugs (like a blood pressure pill that includes a diuretic).
- Reducing frequency-switching from three times a day to once a day, using longer-acting versions of the same medicine.
- Combining both-fewer pills, fewer times. This is the most powerful approach.
Studies show that 41% to 56% of older adults’ medication regimens can be simplified. In aged care homes in Australia, pharmacists using the MRS GRACE tool found that nearly 60% of residents had regimens that could be made easier. And here’s the kicker: when simplification happens, adherence goes up. People remember to take their meds. They feel less stressed. They stay independent longer.
How It Works: The 5-Step Process
Simplifying meds isn’t a quick fix. It’s a careful process. Here’s what it looks like in practice:
- Get the full picture-Start with a "best possible medication history." That means gathering every drug the person is taking, including over-the-counter pills, vitamins, and herbal supplements. Often, the list from the GP doesn’t match what’s actually in the medicine cabinet. One study found an average of six discrepancies per person.
- Check what’s still needed-Not every pill is still useful. Some were prescribed years ago and aren’t helping anymore. Others interact badly. This is called deprescribing. A pharmacist or doctor reviews each drug: Is it still helping? Is the risk bigger than the benefit? For example, a 90-year-old with mild arthritis might not need a daily NSAID if the pain is under control.
- Look for simplification opportunities-Are there drugs that can be switched to once-daily versions? Can two pills be replaced with a combination tablet? Are there long-acting injectables that reduce the need for daily injections?
- Match timing to daily life-If someone eats breakfast at 8 a.m. and naps at 2 p.m., schedule doses around those times. If a family member visits at 5 p.m., that’s a perfect time to hand out a dose. Simplification isn’t just clinical-it’s practical.
- Check in and adjust-Simplification isn’t a one-time event. After three months, check if the person is taking the meds, if they feel better, and if any side effects popped up. Adjust as needed.
The MRS GRACE tool, developed in Australia, guides pharmacists through five key questions:
- Can dosing times be reduced?
- Are there combination products available?
- Can long-acting formulations be used?
- Are there therapeutic equivalents with simpler regimens?
- Does the patient’s routine support the current schedule?
Training for this takes just two hours. But time is the biggest barrier. A full review can take 45 to 60 minutes per person. Most GPs don’t have that kind of time. That’s why pharmacists are often the key players.
What Works Best-and What Doesn’t
Not all medications respond the same way to simplification. Some benefit hugely. Others don’t.
Great candidates for simplification:
- Antihypertensives-Many blood pressure pills now come in once-daily forms. Switching from twice-daily to once-daily improved adherence by 30% in one Australian study.
- Diabetes meds-Long-acting insulins (like glargine or degludec) can replace multiple daily injections. For some, this cuts from four shots to one.
- Antipsychotics-Oral versions can be replaced with monthly injections, eliminating daily pill-taking.
- Statins-Most are already once-daily. But if someone’s on multiple cholesterol drugs, combining them into one tablet helps.
Tricky cases:
- Thyroid medication-Levothyroxine must be taken on an empty stomach, usually first thing in the morning. You can’t move it to bedtime. Simplification here means fewer other pills around that time, not changing the timing itself.
- Diuretics-If someone takes a water pill, giving it at night means waking up to pee. So it’s usually taken in the morning. Can’t simplify that without causing sleep disruption.
- Medicines with strict food rules-Some need to be taken with food, others without. Mixing them into one schedule can be tricky.
One study found that for diabetic and hypertensive drugs, combining fewer pills with once-daily dosing didn’t always improve adherence. But for insulin and antipsychotics, it did. Why? Because those regimens were more burdensome to begin with. The bigger the mess, the bigger the win from cleaning it up.
Real Impact: Adherence, Safety, and Independence
Simplification isn’t just about remembering pills. It’s about staying out of the hospital.
In one aged care facility in Perth, staff started using the MRS GRACE tool. Within six months, medication administration errors dropped by 30%. That means fewer wrong doses, fewer falls from dizziness, fewer trips to emergency.
For people living at home, simplification means fewer calls to family members asking, "Did I take my pill?" It means less anxiety. One 82-year-old man told his pharmacist, "I used to dread my pill box. Now I just take my one tablet with breakfast. I feel like I’ve got my life back."
Studies show that when regimens are simplified, self-reported adherence improves-even if lab results don’t always show immediate clinical changes. Why? Because adherence is the first step to better outcomes. You can’t lower blood pressure if you’re not taking the medicine.
And here’s something important: simplification doesn’t mean lowering quality of care. It means removing unnecessary barriers. A 2020 study in the Journal of the American Medical Directors Association found that after simplification, no one’s health got worse. Many felt better.
Who Should Lead This?
It’s not just the doctor’s job. It’s not just the pharmacist’s job. It’s a team effort.
- Pharmacists-They’re the experts in drug interactions, formulations, and timing. They can spot opportunities a GP might miss.
- General Practitioners-They need to refer patients for medication reviews and approve changes.
- Carers and family-They know the daily routine. They can tell you when the person eats, sleeps, and forgets. Their input is critical.
- The person themselves-They need to be part of the decision. "Do you prefer one pill in the morning or two at night?" Their preferences matter.
In Australia, 85% of aged care facilities now use some form of simplification. But only 40% of GPs routinely check for medication complexity when prescribing. That gap needs closing.
Barriers and How to Overcome Them
There are real obstacles:
- Time-A full review takes 45-60 minutes. Most clinics don’t have that slot.
- Training-Only 35% of pharmacy schools teach medication simplification formally.
- Reimbursement-In Australia and the U.S., pharmacists aren’t always paid for these reviews.
- Technology-Many EHR systems don’t flag complex regimens.
But solutions are emerging:
- Electronic tools like Epic’s regimen complexity score automatically flag patients with 10+ daily doses.
- Medicare Advantage plans in the U.S. now incentivize simplification to reduce hospital readmissions.
- Germany pays pharmacists extra for conducting medication reviews.
- University of Sydney is running a trial to prove MRS GRACE reduces errors in aged care-results expected late 2024.
If you’re a family member, ask: "Has my loved one had a full medication review this year?" If you’re a clinician, make time for it. It’s not a luxury. It’s a necessity.
The Bigger Picture
The world is aging fast. By 2050, there will be 1.5 billion people over 65. Most will be on multiple medications. If we don’t fix how we manage them, we’ll drown in hospital admissions, caregiver burnout, and preventable decline.
Simplifying medication regimens isn’t about cutting corners. It’s about cutting clutter. It’s about respecting the dignity of older adults who just want to live their lives without being ruled by a pill schedule.
The tools exist. The evidence is clear. The need is urgent. The next step? Start the conversation.
Can I just stop some of my older parent’s medications myself?
No. Stopping medications without professional guidance can be dangerous. Some drugs need to be tapered slowly, and others may be essential even if they seem unnecessary. Always talk to a pharmacist or doctor first. They can determine what’s safe to stop through a process called deprescribing.
How do I know if a medication can be switched to a once-daily version?
Ask the pharmacist. Many common drugs like blood pressure meds, cholesterol drugs, and antidepressants have once-daily versions. But not all do. For example, some diuretics or antibiotics can’t be changed. A pharmacist can check therapeutic equivalents and see if a switch is safe and effective.
Is it safe to combine pills into one container?
Only if the pharmacist says it’s okay. Some pills shouldn’t be crushed or mixed because they’re time-released or sensitive to moisture. Mixing them could make them less effective or even unsafe. Always use a pill organizer provided by the pharmacy, and confirm with them first.
What if my parent refuses to simplify their regimen?
Respect their concerns. Sometimes, people stick with their routine because it gives them a sense of control. Talk to them about why simplification matters-not just for health, but for peace of mind. Involve them in the decision. Ask what time of day they’d prefer to take pills. Small choices make big differences.
Do I need to see a specialist to get this done?
No. A community pharmacist or your GP can start the process. Many pharmacies offer free medication reviews. Ask for a "medication management review" or "Home Medicines Review" (in Australia). These are often covered by Medicare. You don’t need a referral to ask.
Will simplifying my meds make them less effective?
No-when done correctly, simplification keeps the same clinical effect but makes it easier to take. The goal isn’t to change the dose or weaken the drug. It’s to match the right drug, at the right dose, with the right schedule. Studies show no drop in effectiveness when simplification is done properly.
Next steps: Gather all medications in one place. Write down the times and reasons for each. Call your pharmacist and ask for a medication review. Don’t wait for a crisis. Start now.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.