Metformin & Contrast Dye Safety Checker
This tool helps determine whether you should continue or stop metformin before a procedure with contrast dye based on current medical guidelines.
When you're on metformin for type 2 diabetes and need a CT scan or other imaging test with contrast dye, a simple question can cause real anxiety: Should I stop my metformin? For years, the answer was a blanket yes. But today, that advice is outdated-and in many cases, unnecessary.
Why the Concern Exists
Metformin is one of the most common diabetes medications in the world. Over 150 million prescriptions are filled for it each year in the U.S. alone. It’s cheap, effective, and generally safe. But it’s also cleared from the body almost entirely by the kidneys. That’s where contrast dye comes in. Iodinated contrast dye, used in CT scans and angiograms, can sometimes cause temporary kidney stress. This is called contrast-induced acute kidney injury (CI-AKI). In rare cases, if your kidneys slow down after the scan, metformin can build up in your blood. That buildup, combined with other health problems, can lead to lactic acidosis-a dangerous condition where your blood becomes too acidic from too much lactate. Lactic acidosis doesn’t happen because metformin creates lactate. It happens when your body can’t clear lactate fast enough. Metformin interferes with how cells use oxygen to make energy. When that system gets disrupted, cells switch to a less efficient, anaerobic process that dumps lactate into the bloodstream. If your kidneys aren’t working well, that lactate piles up. And if you’re already sick-dehydrated, in heart failure, or septic-that’s when the risk spikes. The scary part? Lactic acidosis from metformin (called MALA) is extremely rare. Studies show fewer than 10 cases per 100,000 patient-years. That’s less likely than being struck by lightning. But because it can be fatal-up to 40% of severe cases end in death-it’s been treated like a major threat for decades.The Old Rule (And Why It’s Wrong)
Until 2016, the FDA told doctors to stop metformin before any procedure using contrast dye, whether it was a simple CT scan or a complex heart catheterization. Patients were told to skip their metformin for 48 hours before and after the scan, regardless of kidney function. That meant healthy people with normal kidneys were suddenly off their diabetes medication. For someone with type 2 diabetes, even a two-day pause can mean high blood sugar, hospital visits, or even diabetic ketoacidosis. And for what? Evidence showed almost zero cases of lactic acidosis in patients with normal kidney function who got contrast dye while still taking metformin. The old rule wasn’t based on solid data. It was based on fear. And fear led to unnecessary disruption in care.The New Guidelines (And What They Mean for You)
In 2016, the FDA updated its label based on real-world evidence. The new rules are simple, smart, and patient-centered:- If your eGFR (a measure of kidney function) is above 60 mL/min/1.73 m², you can keep taking metformin before and after contrast dye. No pause needed.
- If your eGFR is between 30 and 60, stop metformin at the time of the scan. Restart it only after 48 hours, once your kidney function is checked and stable.
- If your eGFR is below 30, metformin is already not recommended. Don’t start or restart it without a nephrologist’s input.
- If you’re getting contrast dye through an artery (like during a heart catheterization), stop metformin regardless of kidney function. Arterial contrast carries higher risk.
- If you have heart failure, liver disease, severe infection, or drink heavily, talk to your doctor-even if your kidneys look fine.
Who’s Still at Risk?
Even with the new rules, some people need extra caution:- People over 65 with declining kidney function
- Those with congestive heart failure (especially if unstable)
- Patients with active infections or sepsis
- Anyone who’s dehydrated before the scan
- People who drink alcohol regularly
- Those on multiple medications that affect kidney function
What Happens If You Don’t Stop When You Should?
Most people who keep metformin during contrast dye won’t have a problem. But if your kidneys are already struggling and you’re dehydrated or sick, metformin can accumulate fast. Symptoms of lactic acidosis are subtle at first: nausea, vomiting, abdominal pain, fatigue, rapid breathing. Later, you might feel dizzy, confused, or have low blood pressure. If you experience these symptoms after a scan, seek help immediately. Blood tests will show high lactate levels and a low blood pH. Treatment is aggressive: IV fluids, oxygen, and often dialysis to remove metformin and lactate from your blood. The sooner you get treatment, the better your chance of recovery.What About Kidney Testing?
Before any contrast procedure, your doctor should check your eGFR. This is a simple blood test that estimates how well your kidneys filter waste. It’s not just a number-it’s your safety gate. If your eGFR is above 60, you’re good to go with metformin. If it’s below 60, you’ll need to pause and retest after 48 hours. Don’t assume your last kidney test from six months ago still applies. Kidney function can drop quickly, especially if you’re sick or dehydrated.What About Dialysis Patients?
If you’re on dialysis, you’re already managing kidney failure. Metformin is usually avoided in this group because it can’t be cleared effectively. But if you’re on peritoneal dialysis or hemodialysis and your doctor still prescribes it, the timing matters. For patients on intermittent hemodialysis, metformin is typically held on dialysis days and restarted after the session. For those on continuous dialysis (CRRT), metformin clearance is much slower-so dosing needs to be adjusted carefully. Always coordinate with your nephrologist.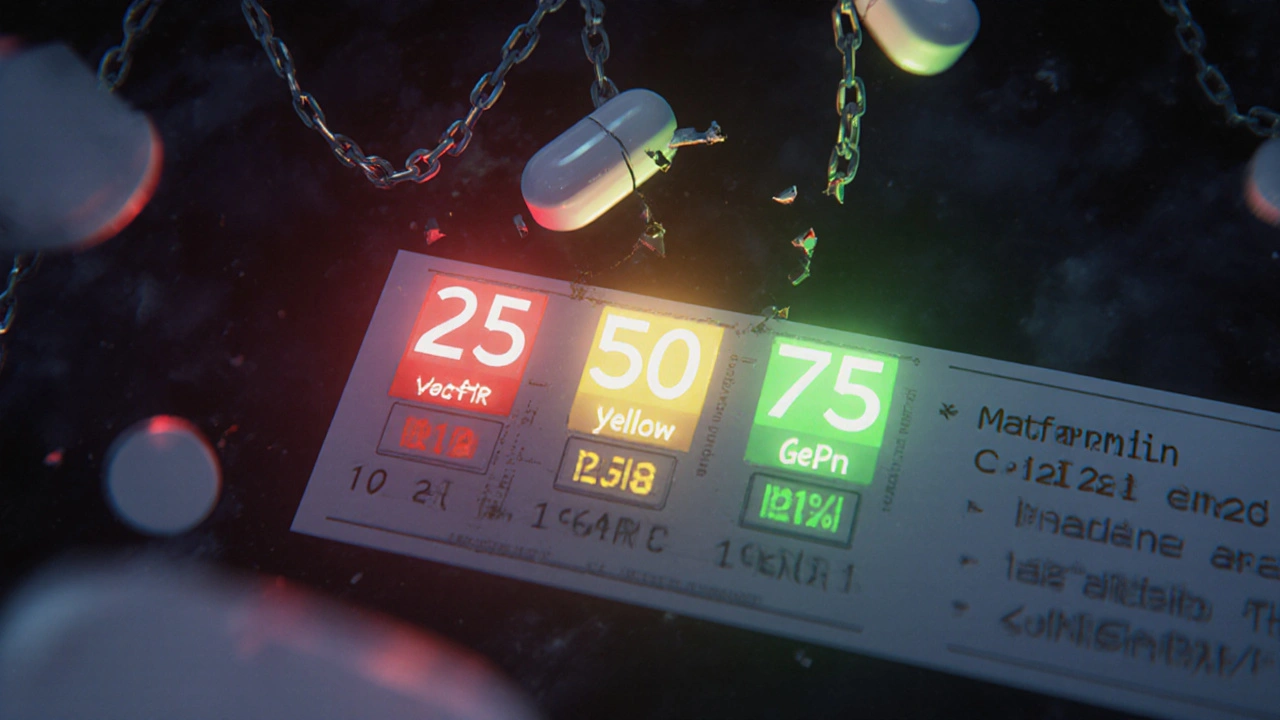
Why This Matters Beyond the Scan
This isn’t just about contrast dye. It’s about how medicine is changing. For years, we treated every diabetic patient the same. Now, we’re learning to personalize care based on real risk-not hypothetical fear. Stopping metformin unnecessarily can cause more harm than the contrast dye ever could. High blood sugar after a scan can lead to infections, longer hospital stays, and even heart problems. The goal isn’t to avoid every possible risk. It’s to avoid the risks that matter.What to Do Next
If you’re scheduled for a scan with contrast dye:- Check your latest eGFR result. If you don’t have one, ask for it.
- Don’t stop metformin unless your doctor tells you to.
- Stay well-hydrated before and after the scan.
- Inform the radiology team you’re on metformin.
- Ask if the contrast will be given intravenously or through an artery.
- Follow up with your doctor 48 hours after the scan to check kidney function if your eGFR is borderline.
Myths vs. Facts
- Myth: Contrast dye always damages kidneys and makes metformin dangerous.
Fact: CI-AKI happens in less than 10% of patients, and only a fraction of those have any risk of lactic acidosis. - Myth: You must stop metformin 48 hours before every scan.
Fact: Only if your eGFR is below 60 or you’re getting arterial contrast. - Myth: Metformin causes kidney failure.
Fact: Metformin doesn’t harm kidneys. It’s cleared by them. That’s why it’s risky if kidneys are already failing. - Myth: Lactic acidosis is common with metformin.
Fact: It’s extremely rare-less than 0.01% of users.
Can I take metformin before a CT scan with contrast dye?
Yes-if your kidney function is normal (eGFR above 60 mL/min/1.73 m²) and you don’t have other risk factors like heart failure, liver disease, or infection. You don’t need to stop it. Always confirm with your doctor, but current guidelines support continuing metformin in these cases.
How long should I wait to restart metformin after a CT scan?
If your eGFR was between 30 and 60 before the scan, wait 48 hours and get a follow-up blood test to check your kidney function. Only restart metformin if your kidneys are working normally. If your eGFR was above 60, you don’t need to stop or restart-it’s safe to continue as usual.
Does contrast dye cause kidney damage in everyone?
No. Contrast-induced kidney injury (CI-AKI) affects only a small percentage of patients, mostly those with pre-existing kidney disease, diabetes, dehydration, or heart failure. For healthy people, the risk is very low. Staying well-hydrated before and after the scan reduces risk even further.
Is lactic acidosis from metformin common?
No. It’s extremely rare-fewer than 10 cases per 100,000 people taking metformin each year. Most cases happen in people with multiple risk factors like kidney failure, severe infection, or heart failure-not from contrast dye alone.
What if I accidentally took metformin before a scan with contrast?
If your kidney function is normal, there’s almost no risk. If your eGFR is below 60, notify your doctor immediately. They may monitor you for signs of lactic acidosis, but most people won’t need treatment. The key is early detection-symptoms like nausea, rapid breathing, or dizziness should be reported right away.
Can I drink alcohol while on metformin before a scan?
It’s best to avoid alcohol for at least 48 hours before and after contrast dye. Alcohol increases the risk of lactic acidosis by affecting liver function and dehydration. Even if your kidneys are fine, combining alcohol with metformin and contrast raises your risk unnecessarily.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.