Why Sarcopenia Is a Silent Threat in COPD
Most people know COPD as a lung disease that makes breathing hard. But what they don’t realize is that up to 22% of COPD patients are also losing muscle - not just from aging, but from the disease itself. This muscle loss is called sarcopenia, and it’s not just about weakness. It’s about survival. People with COPD and sarcopenia are 20-40% more likely to die within five years than those with COPD alone. They get hospitalized more often, can’t walk far, and struggle to do basic tasks like carrying groceries or climbing stairs. And here’s the scary part: many doctors don’t screen for it.
Sarcopenia in COPD isn’t the same as normal aging. In healthy older adults, muscle loss happens slowly, mostly in the legs. In COPD, it hits the chest, arms, and breathing muscles harder. Studies show 68% of COPD patients have noticeably shrunken pectoral muscles - the ones that help you breathe in. That’s nearly three times higher than in people without COPD. The reason? A mix of chronic inflammation, low oxygen at night, not moving enough, and not eating enough protein. It’s a perfect storm.
How Doctors Diagnose Sarcopenia in COPD
There’s no single test. Diagnosis needs three things: low muscle strength, low muscle mass, and poor physical performance. The easiest place to start is with a handgrip strength test. If a man’s grip is under 27 kg or a woman’s under 16 kg, that’s a red flag. Next, they check how much muscle you have. The best way is a DEXA scan, which measures muscle in your arms and legs. For COPD patients, the cutoff is lower than for healthy people: less than 7.0 kg/m² for men, less than 5.5 kg/m² for women.
But here’s the twist: BMI doesn’t work well in COPD. Many patients are thin but still have low muscle mass - a condition called cachexia. That’s why doctors now use something called the pectoralis muscle index (PMI). It measures the size of the chest muscle on a CT scan and adjusts it for body size. A PMI below 1.06 cm²/BMI is a strong sign of sarcopenia in COPD. Physical performance is checked with the Short Physical Performance Battery (SPPB), which looks at balance, walking speed, and chair stands. A score of 8 or lower means you’re in trouble.
These tools aren’t used everywhere. Only 38% of U.S. pulmonary rehab centers screen routinely. That’s changing - but too slowly. If you have COPD and feel weaker than you used to, ask for these tests. Don’t wait until you can’t get out of a chair.
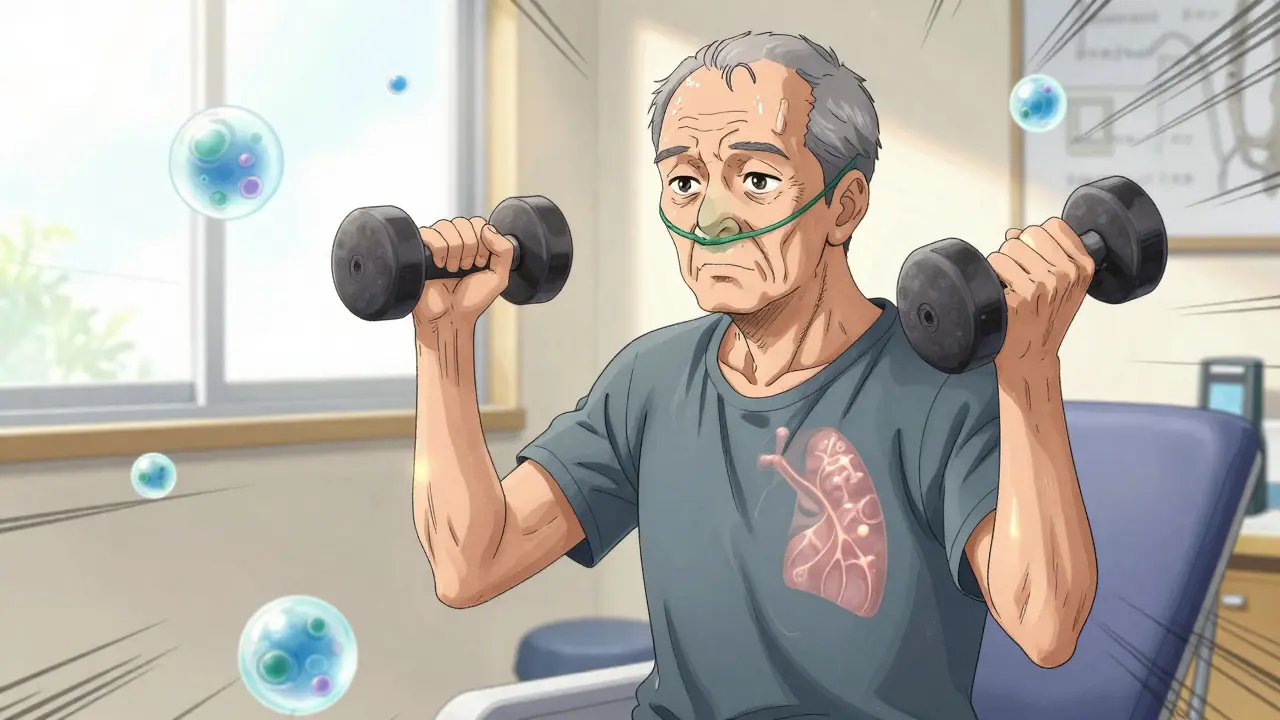
Why Resistance Training Works - Even When Breathing Is Hard
The biggest fear for COPD patients is exercise. They think moving will make them more breathless. But skipping movement makes sarcopenia worse. The good news? Resistance training - even light weights - can rebuild muscle without wrecking your lungs. The key is starting low and going slow.
Studies show that starting at just 30% of your one-rep max (the most weight you can lift once) is safe and effective. That might mean 1- to 2-pound dumbbells or resistance bands. Do 2-3 sessions a week. Focus on big muscle groups: legs, chest, back. Don’t try to lift heavy. Do 10-15 reps per set. Rest 2-3 minutes between sets. That gives your lungs time to catch up.
Here’s what happens when you stick with it: after 12-16 weeks, most people see a 20-25% improvement in how far they can walk. One study at the Cleveland Clinic showed a 23% jump in 6-minute walk distance after 16 weeks of supervised training. That’s not just a number - it’s the difference between needing help to shower and doing it alone.
Some patients need oxygen during training. That’s normal. About 42% of COPD patients with sarcopenia require it. If you’re told to exercise but can’t breathe, ask about supplemental oxygen. It’s not a sign of weakness - it’s part of the plan.
The Protein Problem: Why Most COPD Patients Aren’t Eating Enough
Even the best exercise won’t fix muscle loss if you’re not eating enough protein. The average COPD patient eats about 0.9 grams of protein per kilogram of body weight. The recommended amount for sarcopenia? 1.2 to 1.5 grams per kg. That’s a 30-70% gap.
Why? Loss of appetite. Fatigue. Medications. The simple truth: most people with COPD don’t feel hungry. But muscle repair happens best when protein is spread evenly across meals. Aim for 0.3-0.4 grams per kg per meal - that’s about 20-30 grams of protein per meal for a 70kg person.
Good sources: eggs, lean chicken, fish, Greek yogurt, cottage cheese, tofu, and whey protein. A single scoop of whey protein powder (about 25g protein) can be mixed into a smoothie or oatmeal. Add 2.5-3 grams of leucine per meal - an amino acid that triggers muscle growth. Some supplements include it. If not, look for whey protein with at least 10g leucine per serving.
One patient, Mary Thompson, 68, told the COPD Foundation: “After 12 weeks of protein shakes and light bands, I could carry groceries again.” She didn’t lift heavy. She just ate more protein, consistently, every day.
What Doesn’t Work - And Why
Not all advice for sarcopenia applies to COPD. Standard gym routines? Too intense. High-rep bodyweight exercises? Can trigger breathlessness. Waiting until you feel strong to start? You’ll lose too much muscle.
Some patients try protein powders but don’t use them regularly. Others do resistance training but skip rest days. Muscle grows during recovery - not during the workout. If you’re exhausted after a session, you did too much.
Another myth: “I’m thin, so I don’t need to worry about muscle.” Thin doesn’t mean strong. Many COPD patients are underweight but still have dangerously low muscle mass. That’s sarcopenia. It’s not about weight - it’s about function.
And don’t wait for a flare-up to stop. About 57% of patients quit exercise during COPD exacerbations. That’s a mistake. Even light movement - seated leg lifts, arm circles - helps prevent muscle loss. Talk to your rehab team about safe options during flare-ups.
What’s Changing - And What’s Coming
The field is evolving fast. In 2024, GOLD released the first official algorithm for managing sarcopenia in COPD. It links nighttime oxygen levels to exercise plans. If your oxygen drops below 88% for more than 30% of sleep, your rehab program adjusts. That’s huge - because low oxygen at night directly fuels muscle breakdown.
New drugs are on the horizon. One experimental drug, PTI-501, blocks myostatin - a protein that limits muscle growth. Early trials show promise. Another, HMB (beta-hydroxy-beta-methylbutyrate), is being tested in a major European trial. It’s a natural compound that helps preserve muscle during illness.
But the biggest change isn’t a drug or device. It’s awareness. The number of rehab centers screening for sarcopenia has doubled since 2020. More insurance plans are covering protein supplements and supervised training. By 2027, experts predict managing muscle loss will be as standard as giving oxygen to COPD patients.
What You Can Do Today
Start with two simple steps:
- Ask your doctor for a handgrip strength test and a Short Physical Performance Battery (SPPB). If you score low, ask for a referral to pulmonary rehab.
- Track your protein intake for three days. Use an app like MyFitnessPal. If you’re under 1.2 g/kg/day, add one protein-rich snack or shake per day. Aim for 25-30g protein per meal, spread across 4 meals.
Don’t wait for symptoms to get worse. Muscle loss in COPD is reversible - but only if you act early. The sooner you start, the more independence you keep.
Can sarcopenia be reversed in COPD patients?
Yes, sarcopenia can be reversed - even in advanced COPD. Studies show that combining resistance training with adequate protein intake can increase muscle mass and strength within 12-16 weeks. Patients in pulmonary rehab programs have improved walking distance by 20-25% and reduced hospital visits by 32%. It takes time and consistency, but the results are real.
How much protein should a COPD patient with sarcopenia eat daily?
A COPD patient with sarcopenia should aim for 1.2 to 1.5 grams of protein per kilogram of body weight each day. For a 70kg person, that’s 84-105 grams daily. Spread this across 3-4 meals - about 25-30g per meal - to maximize muscle repair. Adding 2.5-3g of leucine per meal (found in whey protein) boosts muscle synthesis by up to 37%.
Is resistance training safe for someone with severe COPD?
Yes, if done correctly. Start with very light resistance - 1-2 pound dumbbells or resistance bands - and do 10-15 reps per set. Rest 2-3 minutes between sets. Many patients need supplemental oxygen during training; that’s normal and safe. Supervised pulmonary rehab programs are the best way to start. Avoid high-intensity workouts. Progress slowly based on breathlessness, not strength.
Why do COPD patients lose muscle faster than healthy older adults?
COPD patients lose muscle at 3-4 times the rate of healthy aging - about 3.2% per year versus 1-2%. This is due to chronic inflammation (high levels of TNF-α and IL-6), low oxygen levels during sleep, reduced physical activity, and inadequate protein intake. The lungs aren’t the only problem - the whole body is under stress, which accelerates muscle breakdown.
What’s the best way to measure muscle loss in COPD?
The most practical method is handgrip strength and the Short Physical Performance Battery (SPPB). For accurate muscle mass measurement, DEXA scans are best, but they’re not always available. In clinical settings, the pectoralis muscle index (PMI) from a CT scan is more reliable than BMI for COPD patients. A PMI below 1.06 cm²/BMI strongly suggests sarcopenia.
Final Thought: It’s Not Just About Lungs - It’s About Living
Sarcopenia in COPD isn’t an afterthought. It’s a core part of the disease. Treating it isn’t optional - it’s what keeps you independent, mobile, and alive. You don’t need to run a marathon. You just need to lift a little, eat enough protein, and keep going - even on the hard days. The goal isn’t to be strong. It’s to be free.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.