Warfarin Antibiotic Risk Calculator
Antibiotic Interaction Assessment
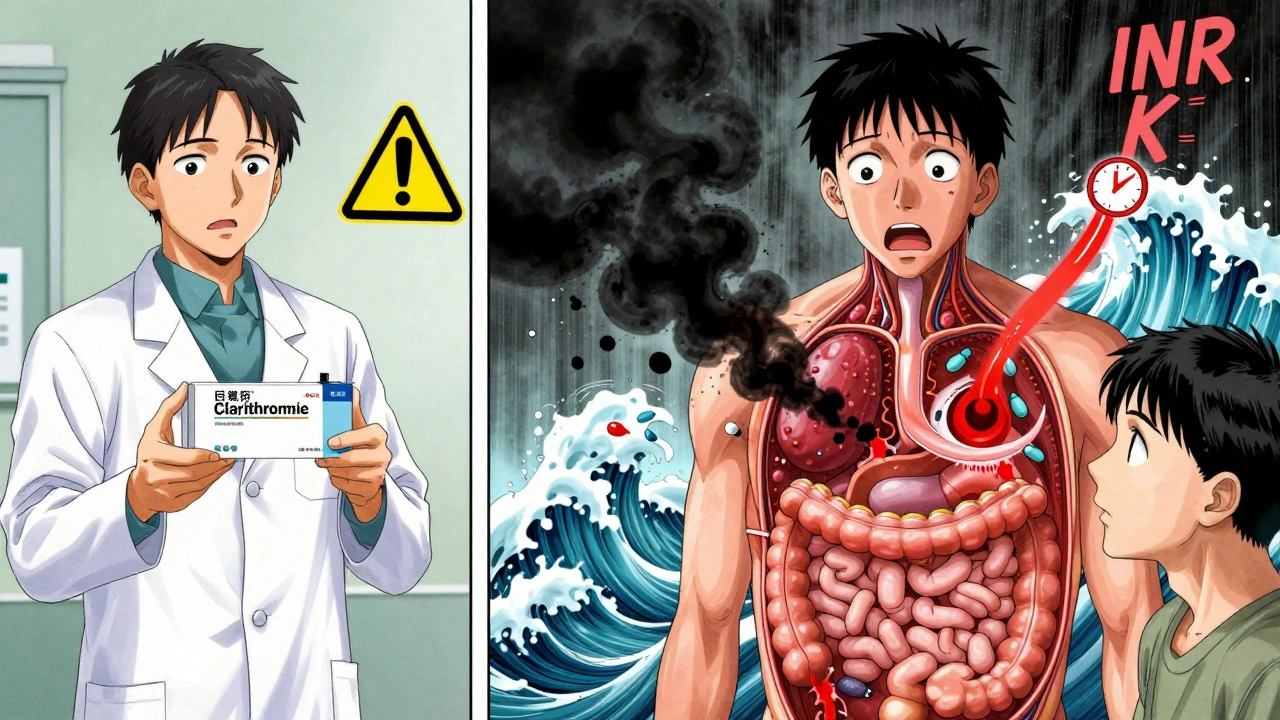
When you're on warfarin, even a simple antibiotic can throw your blood clotting off balance - sometimes dangerously so. It’s not just about taking pills. It’s about how those pills talk to each other inside your body. And when antibiotics meet warfarin, the conversation can turn life-threatening if you’re not paying attention.
Why Warfarin Is So Sensitive
Warfarin isn’t like most medications. It has a razor-thin safety zone. Too little, and you’re at risk of a stroke or pulmonary embolism. Too much, and you could bleed internally - even from a minor bump. That’s why doctors monitor your INR, a standardized number that tells them how long your blood takes to clot. For most people on warfarin, the target is 2.0 to 3.0. Anything above 5.0 is a red flag.What makes warfarin so tricky is how your body handles it. It’s broken down mainly by two liver enzymes: CYP2C9 and CYP3A4. Many antibiotics interfere with these enzymes. Some block them, making warfarin stick around longer. Others change the bacteria in your gut that make vitamin K - the very thing warfarin tries to block. Less vitamin K means stronger anticoagulation. And that’s where INR spikes happen.
Not All Antibiotics Are Created Equal
Some antibiotics barely touch your INR. Others? They’re like a sledgehammer to your anticoagulation control.High-risk antibiotics: These are the ones that most often cause INR to jump 1.5 to 3 points within a week. That’s enough to push someone from a safe 2.5 to a dangerous 5.5.
- Fluoroquinolones - especially levofloxacin and ciprofloxacin - are notorious. One 2023 study found levofloxacin increased bleeding risk by 2.3 times compared to warfarin alone. But here’s the twist: some studies show ciprofloxacin is safer than others. The inconsistency means you can’t assume all fluoroquinolones are equal.
- Macrolides - clarithromycin is a major offender. It blocks CYP3A4 and can raise INR by 2.5 points in over a third of patients. Azithromycin? Almost no effect. So if you need a macrolide, ask if azithromycin is an option.
- Sulfonamides - like trimethoprim-sulfamethoxazole (Bactrim) - hit you with a double punch: they inhibit CYP2C9 and kill vitamin K-producing gut bacteria. INR spikes of 1.2 to 3.0 are common within 4 to 7 days.
- Metronidazole - often used for dental infections or bacterial vaginosis - is another sneaky one. It slows warfarin breakdown and can push INR up by 1.5 to 2.8 points, peaking around day 7.
Low-risk antibiotics: These are usually safe - but not always.
- Penicillins (amoxicillin, ampicillin)
- Cephalosporins (ceftriaxone, cefazolin)
Most people on these won’t see any INR change. But there are exceptions. High-dose IV penicillin has caused spikes in rare cases. So don’t assume safety - just because a drug is labeled "low-risk" doesn’t mean you can skip monitoring.
The Delayed Effect: Why You Can’t Just Check INR the Next Day
Here’s where most people get caught off guard. The INR doesn’t spike right away. It takes 3 to 7 days for gut bacteria to stop making vitamin K. It can take up to 10 days for liver enzyme changes to fully impact warfarin levels.That means if you start an antibiotic on Monday, your INR might look fine on Tuesday. By Friday, it could be climbing. By next Tuesday? It could be over 5.0.
The same thing happens when you stop the antibiotic. Your gut bacteria bounce back. Vitamin K production resumes. Warfarin starts breaking down faster. Your INR can crash - dropping from 2.8 to 1.2 in just a few days. That’s not just a lab number. That’s a real risk of clotting. There are documented cases of strokes happening after antibiotics were stopped and INR wasn’t checked.
Who’s at Highest Risk?
Not everyone on warfarin will have a bad reaction. But some people are far more vulnerable.- Age 75+ - metabolism slows. Drug clearance drops. Risk goes up.
- Cancer patients - their INR is already unstable. Antibiotics push them over the edge. One study found cancer patients were nearly twice as likely to have dangerous INR spikes.
- Women - studies show women have a 42% higher risk than men, likely due to differences in liver enzyme activity and body composition.
- People with baseline INR above 2.5 - they’re already close to the danger zone. A small nudge can send them into the red.
If you fit any of these categories, you need to treat every antibiotic like a potential crisis. No exceptions.
What You Need to Do - Step by Step
If you’re on warfarin and your doctor prescribes an antibiotic, here’s what you must do:- Ask: "Is this antibiotic high-risk for warfarin?" Don’t assume your doctor knows. Bring a list of your meds. Mention warfarin by name.
- Get an INR test before you start. This gives you a baseline. You’ll know how much it changes.
- Test again 3 to 5 days after starting the antibiotic. If it’s a high-risk one, test again at day 7 and day 10.
- Test again 7 to 10 days after stopping. Your INR might drop - and you could be at risk of a clot.
- Watch for signs of bleeding. Unexplained bruising, nosebleeds that won’t stop, dark or bloody stools, headaches, or sudden weakness. These aren’t normal. Call your doctor immediately.
Some patients now use home INR monitors like the Roche CoaguChek INRange. If you have one, use it daily during antibiotic therapy. It’s not a luxury - it’s a lifesaver.
What About Dose Changes?
Should your warfarin dose be lowered when you start an antibiotic? Sometimes. But it’s not one-size-fits-all.For high-risk antibiotics like metronidazole or clarithromycin, reducing your warfarin dose by 25-30% before or right after starting can help prevent spikes. But you can’t guess. That decision needs to be made with your doctor, based on your baseline INR and history.
When you stop the antibiotic, don’t just go back to your old dose. You’ll likely need to increase your warfarin by 15-20% to get back to target. Your INR will drop fast. Waiting too long to adjust can lead to clots.

The Bigger Picture: Why This Still Happens
You’d think this is common knowledge. But it’s not.A 2020 study found only 48% of primary care doctors correctly identified which antibiotics are high-risk. Only 33% consistently ordered INR checks after prescribing them. That’s why 18% of warfarin-related emergencies are tied to antibiotic interactions.
And it’s not just doctors. Patients often don’t know to ask. They take the antibiotic, feel fine, and assume everything’s okay. Then they wake up with a swollen leg or a headache that won’t go away - and it’s too late.
The FDA now requires antibiotic labels to warn about warfarin interactions. But warnings on a label don’t change behavior. Awareness does.
What’s Next?
New tools are helping. Genetic testing can now tell you if you’re a slow metabolizer of warfarin (CYP2C9 variant). That info lets doctors predict how you’ll react to antibiotics before you even take them. The 2022 WARFARIN-ABX trial showed this reduced instability by 37%.AI tools are also getting better. One system, WAR-DRUG, uses your medical history, lab results, and current meds to predict your INR response to specific antibiotics with nearly 90% accuracy.
But the best tool is still you - informed, vigilant, and speaking up. Warfarin isn’t going away. Even with newer drugs like apixaban and rivaroxaban, warfarin is still used by over 3 million Americans because it’s cheap, effective, and works for complex cases.
And as long as antibiotics are prescribed - which they are, often unnecessarily - this interaction will keep happening. The only way to stop it is to treat it like the serious risk it is.
Bottom Line
Warfarin and antibiotics don’t mix casually. Even a "safe" antibiotic can trigger a bleeding crisis - or a clot - if you’re not watching your INR. The key isn’t avoiding antibiotics. It’s knowing which ones are dangerous, when to test, and how to respond. Don’t wait for symptoms. Don’t assume your doctor will catch it. Take control. Get tested. Speak up. Your life depends on it.Can I take amoxicillin while on warfarin?
Most people can take amoxicillin safely while on warfarin. It rarely affects INR - less than 5% of users see any change. But it’s not zero risk. Always check your INR before starting and again 5 days later, especially if you’re older, have cancer, or your INR is already high. Don’t skip monitoring just because it’s "low-risk."
How long after stopping an antibiotic should I check my INR?
Check your INR 7 to 10 days after stopping any antibiotic that affected your INR. When you stop, your gut bacteria start making vitamin K again, and your liver starts breaking down warfarin faster. Your INR can drop quickly - sometimes from 2.8 to 1.2 in just 4 days. That puts you at risk for clots. Don’t wait for symptoms.
Is azithromycin safe with warfarin?
Yes, azithromycin is generally safe with warfarin. Unlike clarithromycin, it doesn’t inhibit liver enzymes and doesn’t affect gut bacteria in a way that lowers vitamin K. Studies show no significant INR changes in over 98% of patients. If you need a macrolide, azithromycin is your best bet.
Why does my INR go up even if I’m taking the same dose?
It’s not just about the dose. Warfarin’s effect depends on how your body processes it - and that changes with antibiotics, diet, illness, or even travel. Antibiotics can block liver enzymes or kill vitamin K-producing bacteria. Even a mild cold or flu can alter your INR. That’s why regular testing is non-negotiable - not just when you start a new drug.
What should I do if my INR is over 5.0?
If your INR is over 5.0, contact your doctor immediately. You may need vitamin K (oral or IV) to bring it down fast. Avoid aspirin, NSAIDs, or alcohol - they increase bleeding risk. Don’t wait for bruising or bleeding. High INR can cause internal bleeding without symptoms. Your doctor will likely pause warfarin and retest in 24-48 hours.
Can I use a home INR monitor during antibiotic therapy?
Yes - and it’s strongly recommended if you’re on a high-risk antibiotic. Devices like the Roche CoaguChek INRange let you test daily. You’ll catch spikes early, avoid hospital visits, and give your doctor real-time data to adjust your dose safely. Many patients on warfarin with complex needs are now using them during antibiotic courses.


Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.