Medication Side Effect Emergency Kit Checklist
Antihistamines (e.g., Benadryl)
For itching, hives, mild swelling from allergic reactions
Hydrocortisone cream (1%)
For skin rashes and irritation
Antacids (e.g., Tums)
For stomach upset, heartburn, nausea
Loperamide (Imodium)
For sudden diarrhea (especially after antibiotics)
Epinephrine auto-injector (EpiPen)
For severe allergic reactions (only if prescribed)
Emergency contact list
Poison control (1-800-222-1222), doctor, pharmacist, 911
Medical records folder
Current meds, allergies, medical history
Special needs items
(Customized based on household type)
Never use expired medications. Keep all supplies in original packaging with expiration dates visible. Store in a cool, dry place away from bathrooms and car interiors.
Why You Need a Home Emergency Kit for Medication Side Effects
Most people keep a first-aid kit for cuts, burns, or sprains. But what about when a pill causes a rash, nausea, or trouble breathing? Medication side effects are common - and sometimes dangerous. In the U.S., over 1.5 million people are harmed each year by medication errors or unexpected reactions. You don’t need to wait for an ambulance if you’re prepared. A targeted home emergency kit for medication side effects can buy you critical time - and possibly save a life.
What Goes in the Kit? Core Supplies for Common Reactions
This isn’t your average first-aid box. It’s built for the specific risks of drugs you or your family take daily. Start with these essentials:
- Antihistamines like diphenhydramine (Benadryl): For itching, hives, or mild swelling from allergic reactions. About 5-10% of people have some kind of reaction to medications, and antihistamines are the first line of defense.
- Hydrocortisone cream (1%): For skin rashes, redness, or irritation. Drug-induced rashes are one of the most frequent side effects - often mistaken for a virus or bug bite.
- Antacids like calcium carbonate or magnesium hydroxide: To calm stomach upset, heartburn, or nausea. Up to 30% of people on certain medications report gastrointestinal issues. Take them at the first sign of discomfort - don’t wait.
- Loperamide (Imodium): For sudden diarrhea, especially after starting antibiotics. About 25% of antibiotic users get this side effect. Keep a small bottle handy.
- Epinephrine auto-injector (EpiPen): Only if prescribed. If you or someone in your home has a history of severe allergies to medications, this isn’t optional. Anaphylaxis can start in minutes. Having it ready means you won’t lose precious seconds.
Don’t forget pain relievers - but be careful. Acetaminophen (Tylenol) is common, but taking it on top of another medicine that already contains it can lead to liver damage. Over 56,000 ER visits each year are from accidental acetaminophen overdose. Always check labels.
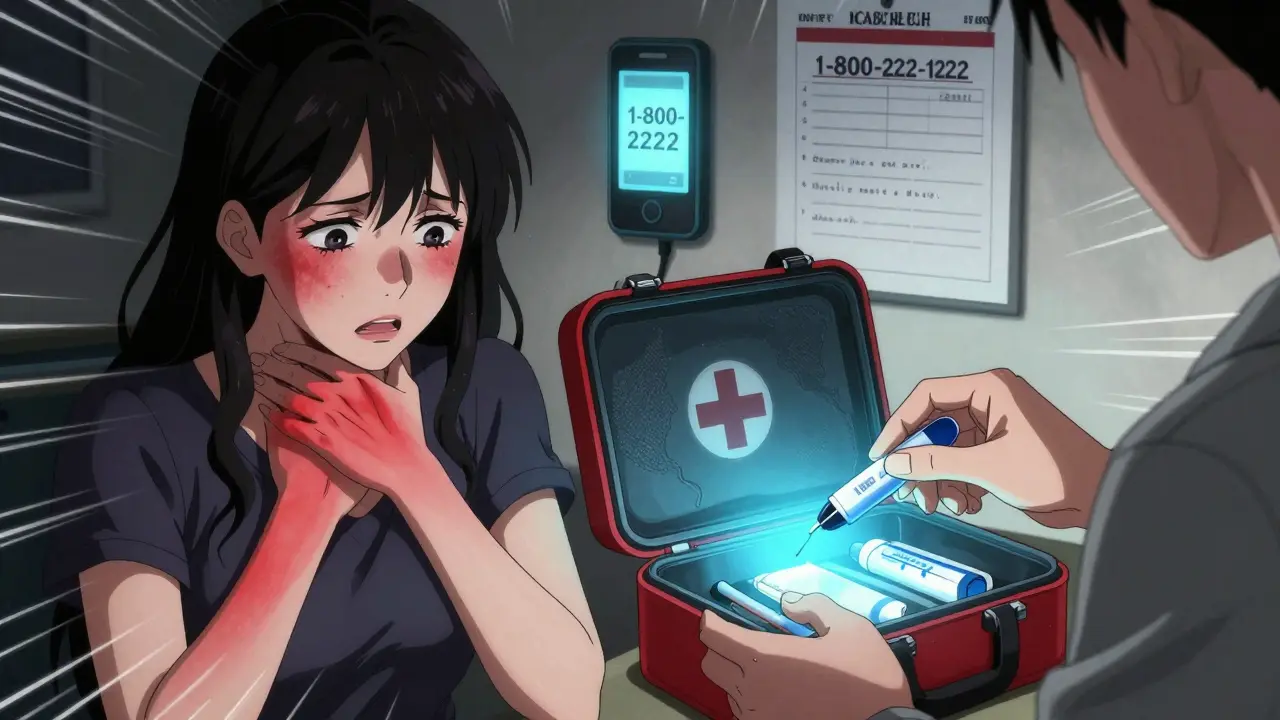
Emergency Contacts: Your Lifeline When Things Go Wrong
Knowing what to do is useless if you can’t get help fast. Your kit must include a printed list of contacts, not just saved on your phone. Power outages, dropped calls, or panic can make digital access unreliable.
- Local poison control: In the U.S., call 1-800-222-1222. It’s free, 24/7, and staffed by toxicology experts. They’ve handled over 2 million cases in 2022 - 11% were from medications.
- Your primary doctor and pharmacist: Keep their direct numbers. Pharmacists know your full medication history and can advise instantly.
- Pediatrician (if you have kids): Never give aspirin to children. It can cause Reye’s syndrome, a rare but deadly condition. For fever or pain, use acetaminophen or ibuprofen instead - and know the right dose by weight.
- Emergency services: 9-1-1 or your local emergency number. Use this for chest pain, trouble breathing, loss of consciousness, or swelling of the throat. The kit helps stabilize - it doesn’t replace 911.
Medical Records: The Most Important Item in the Kit
A list of medications isn’t enough. You need full medical profiles for every person in your household. Include:
- Current prescriptions, doses, and frequency
- All known drug allergies (even mild ones like “rash from penicillin”)
- Previous adverse reactions - what happened, when, and how it was treated
- Chronic conditions: diabetes, heart disease, epilepsy, etc.
- Any recent changes in meds - doctors often miss these during emergencies
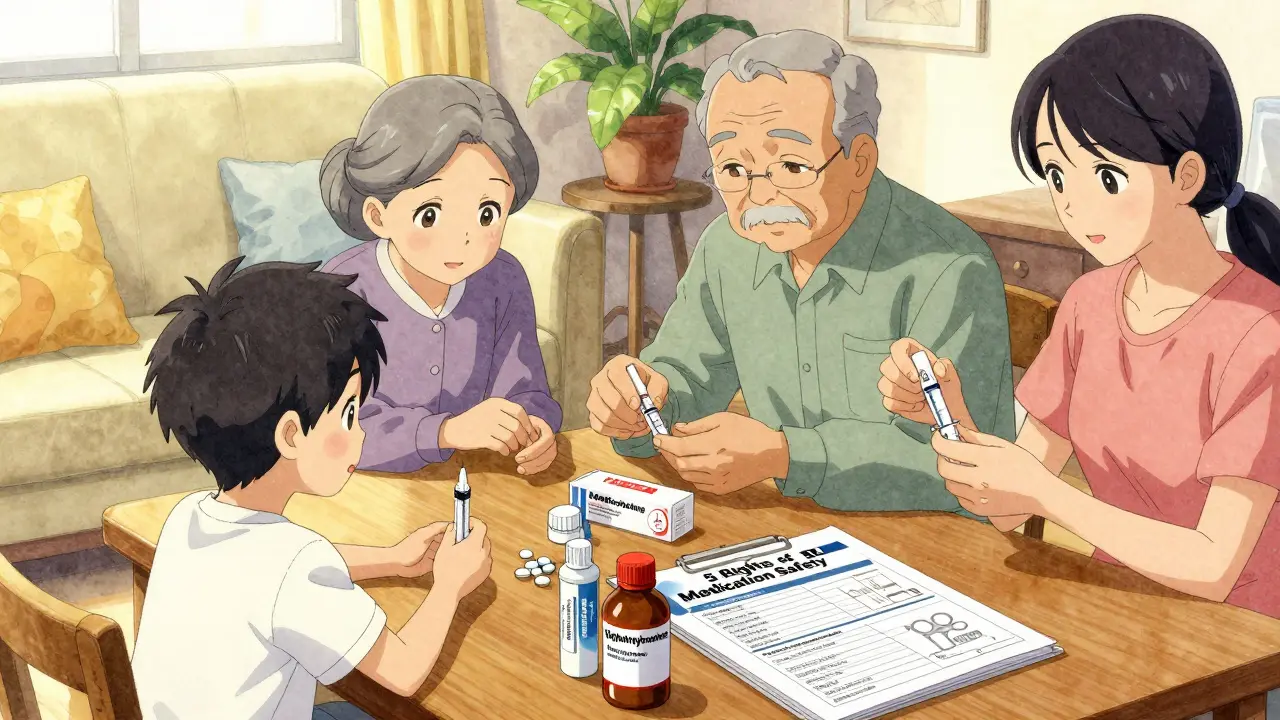
Use the 5 Rights of Medication Safety as your checklist: right patient, right drug, right dose, right route, right time. Write this on the front of the folder. In an emergency, paramedics or ER staff will scan this first. Detailed records improve diagnosis accuracy by up to 40%.
Special Needs: Kids, Seniors, and Chronic Conditions
One size doesn’t fit all. Your kit should adapt to who’s in your home.
For children: Skip aspirin entirely. Use weight-based doses of acetaminophen (10-15 mg/kg) or ibuprofen (5-10 mg/kg). Keep a small syringe or dosing cup in the kit. Store all meds out of reach - over 60,000 kids are treated yearly for accidental poisoning.
For seniors: Most take 4-5 prescriptions daily. Include a printed weekly schedule with large print. Add a pill organizer if needed. Watch for interactions - many side effects in older adults are missed because they’re blamed on aging.
For diabetics: If you take insulin or other blood sugar-lowering meds, include glucose tablets or juice boxes. Low blood sugar from drug interactions can happen fast. Don’t wait for dizziness - treat it immediately.
Storage and Maintenance: Don’t Let Your Kit Go Bad
Expired meds are useless. Poorly stored meds can lose potency. Check your kit every three months.
- Store in a cool, dry place - not the bathroom or car. Heat and moisture ruin pills and creams.
- Keep everything in original packaging. Labels have expiration dates, dosing info, and warnings.
- Replace anything expired. The FDA says potency drops over time - sometimes by 10-50% before the date even passes.
- Test battery-powered items like flashlights or auto-injector trainers. A dead battery won’t help in a crisis.
- Write the date you last checked on the outside of the kit.

What NOT to Include
Some things sound helpful but aren’t. Avoid:
- Activated charcoal: Older guides recommended it for poisonings, but experts now say it doesn’t work for most medications. Leave it to professionals.
- Unprescribed antibiotics or steroids: These can mask symptoms or cause worse reactions. Never guess.
- Leftover pills from old prescriptions: Even if they look fine, they’re not safe to reuse. Dispose of them properly.
How to Use the Kit - Step by Step
When a side effect happens:
- Stop the medication immediately - unless told otherwise by a doctor.
- Call poison control (1-800-222-1222) or your pharmacist. They’ll tell you what to do next.
- If it’s mild (rash, nausea), use the kit supplies as directed.
- Write down what happened: time, symptoms, what you took, what you did. Use the notepad in your kit.
- If symptoms worsen - chest pain, swelling, trouble breathing - call 9-1-1. Don’t wait.
Remember: This kit is for stabilization, not cure. Its job is to keep someone safe until professional help arrives.
Get Started Today
You don’t need to buy everything at once. Start with the top three: antihistamines, antacids, and emergency contacts. Add one item each week. Talk to your pharmacist - they’ll help you pick the right brands and doses. Most will even give you a free printed list of your meds.
Every household with medication users needs this. It’s not about fear. It’s about control. When you’re prepared, you’re not helpless.
Can I use over-the-counter meds for any side effect?
No. Some OTC meds can interact dangerously with your prescriptions. For example, taking ibuprofen with blood pressure meds can raise kidney risk. Always check with your pharmacist before using anything new, even if it’s sold without a prescription.
Do I need an EpiPen if I’ve never had a severe reaction?
Only if your doctor prescribes it. Most people won’t need one. But if you’ve had swelling, trouble breathing, or a drop in blood pressure after a medication, talk to your doctor about whether you should carry one. Don’t guess - get it checked.
How often should I check my emergency kit?
Every three months. That’s when you should check expiration dates, replace used items, and update your medical list. Set a reminder on your phone for the first day of each season - it’s easy to remember.
What if I’m traveling with this kit?
Take a smaller version with you. Keep antihistamines, antacids, and your emergency contact list in your carry-on. Never check it in luggage. If you’re flying, keep medications in original bottles with your name on them. You may be asked to show them at security.
Can I make a kit for my pet?
No. Human meds can be deadly for pets. Even a single tablet of ibuprofen or acetaminophen can poison a dog or cat. If your pet has a reaction to a vet-prescribed drug, call your vet or an animal poison control center immediately. Never give human meds to animals.
Is this kit covered by insurance?
Usually not. But some health savings accounts (HSAs) or flexible spending accounts (FSAs) may allow you to use pre-tax dollars to buy items like antihistamines, hydrocortisone cream, or glucose tablets. Check with your provider. Even if it’s not covered, the cost is low - under $50 for a basic kit.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.