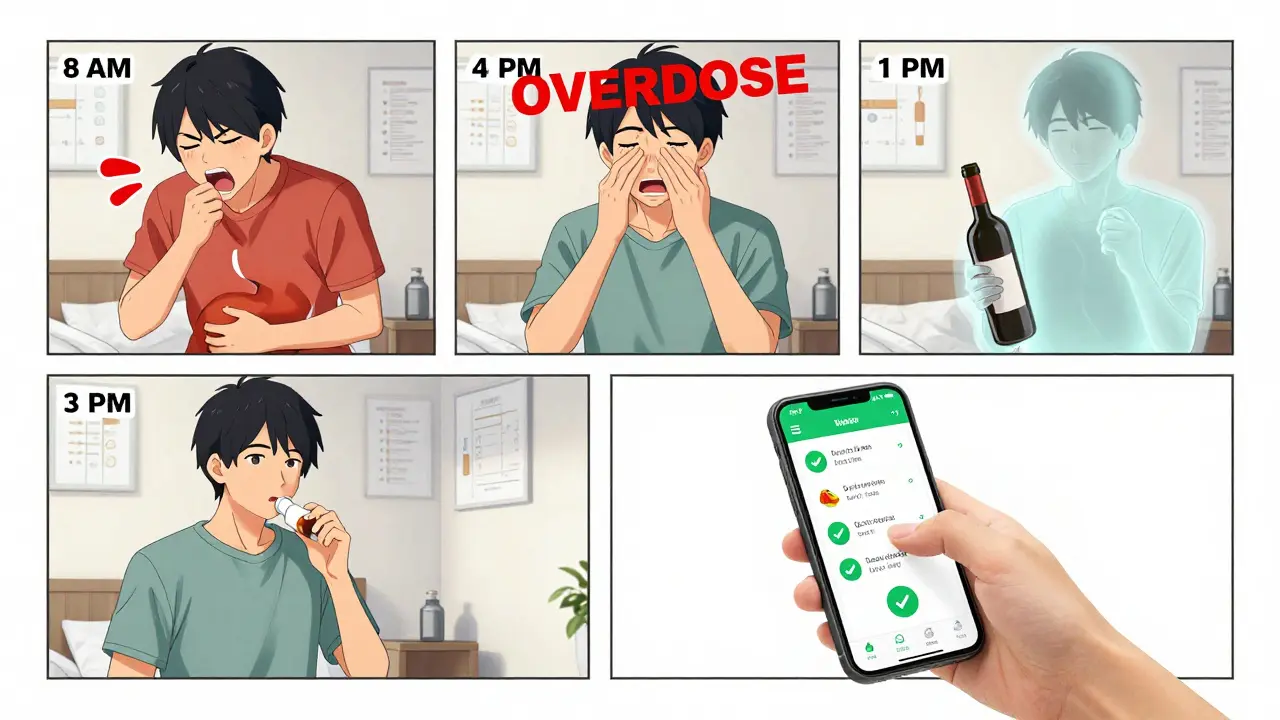
Getting your medication schedule right isn’t just about setting an alarm. It’s about understanding what’s written on the label - and using that information to build reminders that actually keep you safe. Too many people miss doses or take pills at the wrong times because they’re relying on simple alarms that ignore the fine print. But the details on your prescription label - the timing, the food warnings, the interactions - are there for a reason. Ignoring them can lead to side effects, reduced effectiveness, or even dangerous overdoses.
What’s Really on Your Prescription Label?
Your medication label isn’t just a receipt. It’s a clinical instruction sheet. The FDA requires specific information to be printed clearly: the name of the drug, the strength (like 10 mg or 500 mg), how often to take it, and special instructions. These aren’t suggestions. They’re safety rules.Look for phrases like:
- "Take one tablet every 8 hours" - that means three times a day, evenly spaced.
- "Take with food" - skipping this can cause stomach upset or reduce absorption.
- "Take on an empty stomach" - eating too soon can make the drug less effective.
- "Do not take more than one dose in 6 hours" - this prevents overdose.
- "Avoid alcohol" or "May interact with blood pressure meds" - these warn about dangerous combinations.
A 2023 NIH study found that 78.3% of timing-related medication errors happen because people don’t follow these label details. If your reminder app just says "Take pill at 8 AM," but the label says "Take with breakfast," you’re missing half the instructions.
Why Basic Alarm Apps Fail
Most free reminder apps - the ones that just beep at set times - don’t understand medication labels. They treat every pill the same. That’s dangerous.Imagine you’re on three medications:
- Warfarin - needs to be taken at the same time every day, no exceptions.
- Metformin - must be taken with meals to avoid low blood sugar.
- Atorvastatin - works best taken at night.
A basic app might remind you to take all three at 8 AM. But if you take metformin without food, you could get dizzy. If you take warfarin at different times, your blood clotting levels become unstable. If you take atorvastatin in the morning, it’s less effective.
Apps like Medisafe and MyTherapy don’t just remind you. They read your label. They know that "every 8 hours" means 8 AM, 4 PM, and midnight - not 8 AM, 12 PM, and 4 PM. They know that if you’re taking two drugs that interact, they need to be spaced two hours apart. They adjust for you.
How Advanced Systems Use Label Data
Modern medication apps use three key technologies to turn labels into smart reminders:- OCR (Optical Character Recognition) - you snap a photo of your pill bottle, and the app reads the text. Modern systems get 98.7% accuracy, even on small print.
- Drug Databases - they compare your meds against 150,000+ drugs and 500,000+ known interactions. If your label says "avoid grapefruit," the app flags it.
- Rule Engines - they convert phrases like "take every 12 hours" into actual times, and then check if those times conflict with other meds.
For example, if your label says "Take one capsule twice daily, with food," the app doesn’t just set two alarms. It sets them 12 hours apart, and then adds a note: "Take with breakfast and dinner." It might even suggest you eat a small snack if you forget lunch.
A 2024 study in the Journal of Medical Systems showed these smart systems reduce timing errors by 63.2% compared to basic alarms. Patients using them had an 82.4% adherence rate - meaning they took their meds correctly more than 8 out of 10 times.
What to Watch Out For
Even the best apps can stumble. Here are the most common pitfalls:- Ambiguous labels - some older or generic meds say things like "take as needed" or "take daily" without specifying time. These require manual input.
- Personal adjustments - your doctor might tell you to take your blood pressure med at 7 PM instead of 8 AM because you work nights. Labels don’t reflect that. Always override the app if your doctor gives you different instructions.
- Time zone changes - if you travel, make sure your app updates to local time. Missing a dose because your phone didn’t adjust is a common mistake.
- Over-reliance - apps aren’t perfect. A 2024 Consumer Reports review found that 14.3% of errors in digital tools came from automated label misinterpretation. Always double-check the app’s schedule against your physical label.
Senior patients benefit the most from this system. A 2024 AARP survey showed 76.4% of adults over 65 understood their medication schedule better when reminders included phrases like "take with breakfast" instead of just "8 AM." Visual timelines - showing when each pill goes in - help too.
How to Set It Up Right
If you’re using a smart medication app, here’s how to make sure it works:- Take a clear photo of every pill bottle. Make sure the label is fully visible, no glare.
- Review the auto-generated schedule - does it match what your doctor told you? Does it respect "with food" or "on empty stomach"?
- Check for interaction warnings - if the app flags a conflict, don’t ignore it. Talk to your pharmacist.
- Update when your prescription changes - even if you just get a refill, the strength or timing might be different.
- Use the notes section - add reminders like "Take with water," "Don’t crush," or "Call doctor if rash appears."
For complex regimens, consider apps that let you share your schedule with a family member or caregiver. That way, someone else can check if the app made a mistake.

The Bigger Picture
This isn’t just about convenience. The Institute of Medicine estimated that poor medication adherence causes 1.5 million preventable injuries and deaths every year in the U.S. alone. In Australia, the Therapeutic Goods Administration reports similar figures - and the problem is growing as more people take multiple medications.By 2026, Medicare and other major health systems will require all digital tools to use label-based scheduling. That’s because the data proves it works. A 2024 Health Affairs study found that systems combining label interpretation with pharmacist review hit 85.1% adherence - the highest rate ever recorded.
It’s not about replacing your doctor. It’s about giving you a tool that respects the science on your label. When your reminder system understands that "take every 6 hours" means 8 AM, 2 PM, 8 PM - not 8 AM, 12 PM, 4 PM - you’re not just following instructions. You’re protecting your health.
Can I just use my phone’s alarm app for medication reminders?
You can, but it’s risky. Basic alarms don’t understand food requirements, drug interactions, or minimum intervals between doses. If your label says "take every 8 hours," a simple alarm might remind you at 8 AM, 12 PM, and 4 PM - which is only 4 hours apart. That could lead to overdose. Smart apps use label data to space doses correctly.
What if my prescription label is hard to read?
Don’t guess. Take a photo and ask your pharmacist to clarify. Many apps use OCR to read labels, but if the print is faded or smudged, they might misread it. Always compare the app’s schedule to the original label. If you’re unsure, call your pharmacy - they’re required to explain your prescription.
Do I still need to check the label if I use a smart app?
Yes. No app is 100% perfect. A 2024 review found that 14.3% of digital errors came from misinterpreted labels. Always review the app’s schedule against your physical label at least once a week. If the app says "take with food" but your label says "take on empty stomach," trust the label and override the app.
What if I take medications from different pharmacies?
That’s common - and it’s why you need a centralized app. Apps like Medisafe and CareZone let you add all your prescriptions, even from different pharmacies. They check for interactions across all your meds, no matter where you got them. Always upload every label, even if it’s a new one.
Can these apps help with complex regimens like insulin or blood thinners?
Yes - and they’re critical. For insulin, timing relative to meals matters. For blood thinners like warfarin, consistency in timing is vital. Smart apps use label data to lock in exact times and flag deviations. Some even sync with glucose monitors or INR trackers. But always confirm with your doctor - these apps support, not replace, medical advice.
Next Steps
If you’re not using a smart medication app yet, start today. Pick one that lets you scan your labels - Medisafe, MyTherapy, or CareZone are good options. Take photos of all your current prescriptions. Review the schedule it creates. Talk to your pharmacist if anything seems off. And never skip checking the label - even with the best tech, your eyes are still the final safety check.Medication safety isn’t about remembering to take a pill. It’s about taking it the right way - at the right time, with the right food, and without dangerous interactions. Your label holds the key. Use it.


Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.