What Is Pleural Effusion?
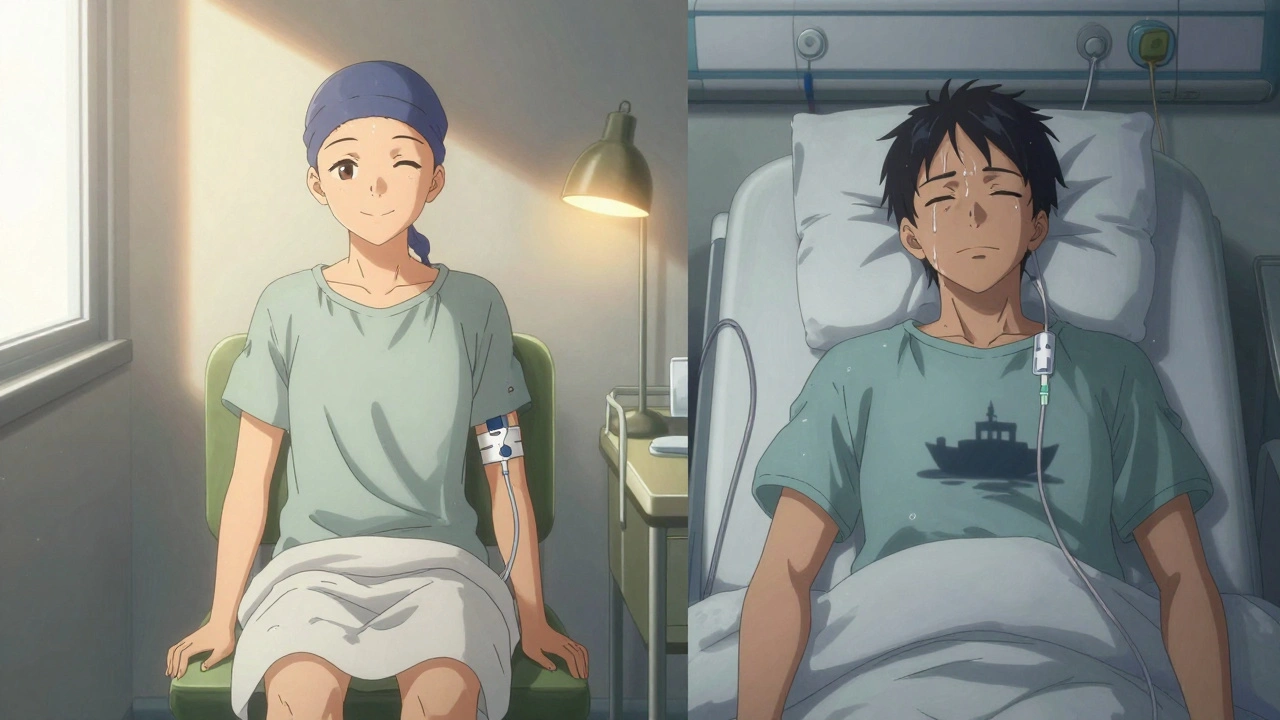
When fluid builds up between the layers of tissue lining your lungs and chest wall, that’s called a pleural effusion. It’s not a disease on its own-it’s a sign something else is wrong. Think of it like swelling around your lungs. That extra fluid makes it harder for your lungs to expand fully, which is why people often feel short of breath, especially when lying down or moving around. Some also get a sharp chest pain when they breathe in, or a dry cough. It’s not always obvious at first, but if you’ve been feeling unusually winded for no clear reason, it’s worth checking.
Every year, about 1.5 million people in the U.S. are diagnosed with this condition. The most common cause? Congestive heart failure. It accounts for nearly half of all cases. But there are many others: pneumonia, cancer, liver disease, kidney problems, and even blood clots in the lungs. The key is figuring out which one is behind the fluid buildup-because treating the effusion alone won’t fix the real problem.
Transudative vs. Exudative: Two Different Kinds of Fluid
Not all pleural effusions are the same. Doctors split them into two main types based on what’s in the fluid and why it’s there.
Transudative effusions happen when fluid leaks through healthy blood vessels because of pressure changes or low protein levels. This type is usually tied to heart failure, cirrhosis, or nephrotic syndrome. In fact, heart failure causes about 90% of these cases. The fluid here is mostly water with low protein and few cells. It’s like water seeping through a leaky pipe-no inflammation, just physics.
Exudative effusions are more serious. They happen when the lining around the lungs gets inflamed or damaged. This could be from pneumonia (which causes 40-50% of exudative cases), cancer (25-30%), pulmonary embolism, or tuberculosis. The fluid is thicker, richer in protein and white blood cells, and often shows signs of infection or cancer cells. Light’s criteria-named after the doctor who developed them in 1972-are used to tell these apart. If the fluid’s protein level is more than half of the blood’s, or if the LDH enzyme is too high, it’s likely exudative. These numbers are accurate 99.5% of the time.
When and How Is Thoracentesis Done?
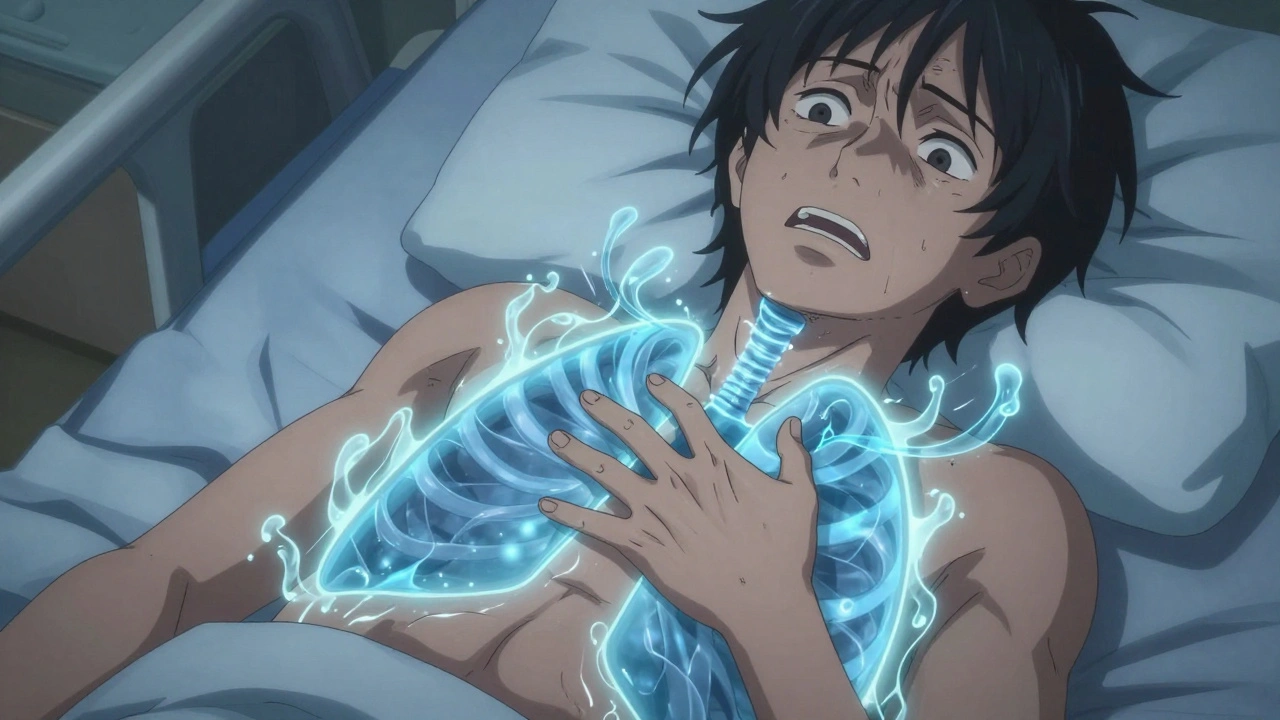
If your doctor suspects a pleural effusion, the first step is often an ultrasound. It’s quick, safe, and shows exactly how much fluid is there. If the fluid is more than 10mm thick, or if you’re having trouble breathing, they’ll likely recommend thoracentesis-a simple procedure to drain the fluid.
The procedure is done with ultrasound guidance, which has become the standard of care. Without it, complications like a collapsed lung (pneumothorax) happen in nearly 19% of cases. With ultrasound, that drops to under 5%. A thin needle or catheter is inserted between your ribs, usually around the 5th to 7th space on your side, and fluid is pulled out. For diagnosis, they take just 50-100 milliliters. For relief, they can remove up to 1,500 milliliters in one session.
The fluid is sent for testing: protein, LDH, cell count, pH, glucose, and cytology. Low pH (below 7.2) or low glucose suggests infection. High LDH (over 1,000 IU/L) can point to cancer. Cytology finds cancer cells in about 60% of malignant cases. If you’ve had recent heart surgery and the fluid keeps coming back, they might also check amylase or hematocrit levels to rule out pancreatitis or blood clots.

What Are the Risks of Thoracentesis?
Most people tolerate thoracentesis well, but it’s not risk-free. About 10-30% of procedures have some kind of complication. The most common is a collapsed lung-this happens in 6-30% of cases without ultrasound, but drops to 2-5% when it’s used. Another rare but serious risk is re-expansion pulmonary edema, where the lung swells up too fast after being compressed for a while. It affects less than 1% of people, but it’s dangerous if missed.
Minor bleeding happens in 1-2% of cases, especially if you’re on blood thinners. That’s why doctors check your clotting status before the procedure. Pain during or after is common but usually mild and short-lived. The big takeaway? Ultrasound isn’t just helpful-it’s essential. Studies show it cuts complication rates by nearly 80%. And if you’re having this done, make sure the person doing it has done at least 25 procedures. That’s the number where skill levels really improve.
Preventing Recurrence: It All Depends on the Cause
Draining the fluid gives you relief-but if you don’t fix what caused it, it will come back. That’s why treatment is always targeted.
For heart failure, the goal is to manage the heart. Diuretics (water pills), ACE inhibitors, and beta-blockers help. When doctors use NT-pro-BNP blood tests to guide treatment, recurrence drops from 40% to under 15% in three months. No need for invasive procedures here-just better medical management.
For pneumonia-related effusions, antibiotics are key. But if the fluid is thick, infected, or has a pH below 7.2 or glucose below 40 mg/dL, you’ll need drainage. Left untreated, 30-40% of these turn into empyema-a pus-filled infection that can be life-threatening. Drainage early prevents that.
For malignant effusions, things get more complex. After draining the fluid, it comes back in about half of patients within 30 days. That’s why doctors move quickly to prevent recurrence. Two main options: pleurodesis or an indwelling pleural catheter.
Pleurodesis involves putting a substance like talc into the chest to irritate the lining and make the two layers stick together. It works in 70-90% of cases. But it’s painful-60-80% of patients report moderate to severe pain afterward. Hospital stays average 5-7 days.
Indwelling pleural catheters are changing the game. These are small tubes left in place for weeks, letting you drain fluid at home. Success rates hit 85-90% at six months, and patients go home the same day. One 2021 study showed hospital stays dropped from 7.2 days to just 2.1 days with this method. For people with advanced cancer who aren’t candidates for aggressive treatment, this is often the best choice.
What Doesn’t Work-and Why
Not every effusion needs drainage. Many small, asymptomatic ones are watched instead. A 2019 study found that 30% of thoracentesis procedures provided no real benefit-no diagnosis, no relief. That’s why guidelines now say: only drain if it’s large enough to cause symptoms or if you need to test it.
Chemical pleurodesis is no longer recommended for non-cancer effusions. There’s no good evidence it helps. And for post-surgery effusions-common after heart bypass-most clear up on their own. If fluid drains more than 500 mL per day for three days straight, then drainage is needed. Otherwise, patience wins.
What’s New in Treatment?
Recent advances are making a real difference. Pleural manometry-measuring pressure inside the chest during drainage-is now used in some centers. Keeping pressure below 15 cm H₂O reduces the chance of re-expansion edema to just 5%. It’s simple, cheap, and effective.
Also, survival for people with malignant effusions has improved. Between 2010 and 2020, 5-year survival jumped from 10% to 25%. Why? Better cancer treatments, earlier detection, and personalized care. If your cancer responds to targeted therapy, your effusion is more likely to stay gone.
The big shift? Treating the cause, not just the symptom. As one expert put it: ‘Treating the effusion without treating the cause is like bailing water from a sinking boat without patching the hole.’
When to Seek Help
If you have unexplained shortness of breath, especially if it’s getting worse, see a doctor. Don’t wait for chest pain or fever. Early diagnosis saves lives. If you’ve had cancer, heart disease, or pneumonia recently and now feel more winded than usual, get checked. A simple ultrasound can rule out or confirm a pleural effusion in minutes.
And if you’ve had a thoracentesis before and the fluid came back, talk to your doctor about long-term options. An indwelling catheter might be better than repeated hospital visits. Don’t assume the only choice is another needle stick.
What causes pleural effusion?
Pleural effusion is caused by fluid leaking into the space around the lungs. The two main types are transudative (from pressure changes, like in heart failure) and exudative (from inflammation or cancer). Common causes include congestive heart failure (50% of cases), pneumonia (40-50% of exudative cases), cancer (25-30%), cirrhosis, kidney disease, and pulmonary embolism.
Is thoracentesis safe?
Yes, when done with ultrasound guidance, thoracentesis is very safe. Complication rates drop from nearly 19% to under 5% when ultrasound is used. The most common risks are a collapsed lung (pneumothorax), minor bleeding, or re-expansion pulmonary edema. These are rare with proper technique and experienced providers.
How do you know if a pleural effusion is cancerous?
Cytology testing of the fluid finds cancer cells in about 60% of malignant cases. High LDH levels (over 1,000 IU/L), low glucose, and low pH also suggest cancer. Imaging and biopsy may be needed if cytology is negative but cancer is still suspected. A diagnosis often requires combining fluid results with scans and clinical history.
Will the fluid come back after thoracentesis?
It depends on the cause. In heart failure, recurrence drops to under 15% with proper treatment. In cancer, it returns in about 50% of cases within 30 days without further treatment. For long-term control, options like indwelling pleural catheters or pleurodesis are used. These reduce recurrence to 10-15% over six months.
What’s the difference between pleurodesis and an indwelling catheter?
Pleurodesis uses chemicals like talc to glue the lung lining to the chest wall, stopping fluid buildup. It’s effective but painful and requires a hospital stay. An indwelling pleural catheter is a small tube left in place so you can drain fluid at home. It’s less invasive, has higher long-term success (85-90%), and lets you go home the same day. It’s now preferred for many cancer patients.
Can pleural effusion be prevented?
You can’t always prevent it, but you can reduce your risk by managing underlying conditions. Control heart failure with medication and diet, treat pneumonia early, avoid smoking, and manage kidney or liver disease. For people with cancer, early intervention with catheters or pleurodesis can prevent repeated hospital visits and improve quality of life.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.