Brand-Name Drugs: What They Are, Why They Cost More, and How They Compare to Generics
When you hear brand-name drugs, original medications developed and marketed by pharmaceutical companies under a proprietary name. Also known as innovator drugs, they’re the first version of a medicine to hit the market after years of research and clinical trials. These are the pills you see advertised on TV—Zestril, Estrace, Unisom, Riluzole—each with a recognizable name and often a higher price tag than what you find at the pharmacy counter.
What makes a drug a brand-name drug, a medication protected by patent and sold under a manufacturer’s trademark. Also known as originator drug, it isn’t just the label. It’s the years of testing, the FDA approval process, and the marketing budget that go into it. Once the patent runs out, other companies can make the same active ingredient—but under a different name. That’s where generic drugs, medications with the same active ingredient, dosage, and effectiveness as brand-name versions, but sold without a brand name. Also known as nonproprietary drugs, they come in. They’re cheaper because they don’t need to repeat expensive trials. The FDA says they work the same. But do they feel the same? Some patients swear there’s a difference. Others save hundreds a month without noticing a thing.
Why does this matter? Because drug pricing, the cost of medications set by manufacturers, insurers, and pharmacies, often influenced by patents and market control. Also known as pharmaceutical costs, it isn’t just about what’s on the shelf—it’s about who can afford it. A 30-day supply of a brand-name drug might cost $300. The generic? $10. For people on fixed incomes, that gap isn’t just a number—it’s whether they take their medicine at all. And it’s not just about money. pharmaceutical patents, legal protections that give companies exclusive rights to sell a drug for a set period, usually 20 years. Also known as drug exclusivity, they keep prices high. When they expire, competition drops costs. But sometimes, companies find ways to extend them—through tiny changes in formulation or delivery—delaying generics for years.
And here’s the thing: not every brand-name drug is worth the extra cost. Some are. Like Riluzole for ALS—there’s still no generic, and it’s the only drug proven to slow progression. But for blood pressure? There are half a dozen generics that work just as well as Zestril. For menopause? Estrace has cheaper alternatives that deliver the same hormones. The real question isn’t whether brand-name drugs are better—it’s whether you’re paying for science, or just for the name.
You’ll find posts here that break down exactly how these drugs compare—why some people react differently to generics, when it’s safe to switch, and how to talk to your doctor about cost without feeling embarrassed. You’ll learn how patent tricks keep prices high, what the FDA really checks in generics, and which brand-name drugs still hold an edge. Whether you’re managing a chronic condition, helping an aging parent, or just trying to stretch your paycheck, this collection gives you the facts—not the sales pitch.
Generics vs Brand-Name Drugs: How Insurance Coverage Policies Really Work
Jan 17, 2026, Posted by Mike Clayton
Learn how insurance formularies treat generic and brand-name drugs differently, why generics cost less, and what to do when you need the brand but your plan won't cover it.
MORE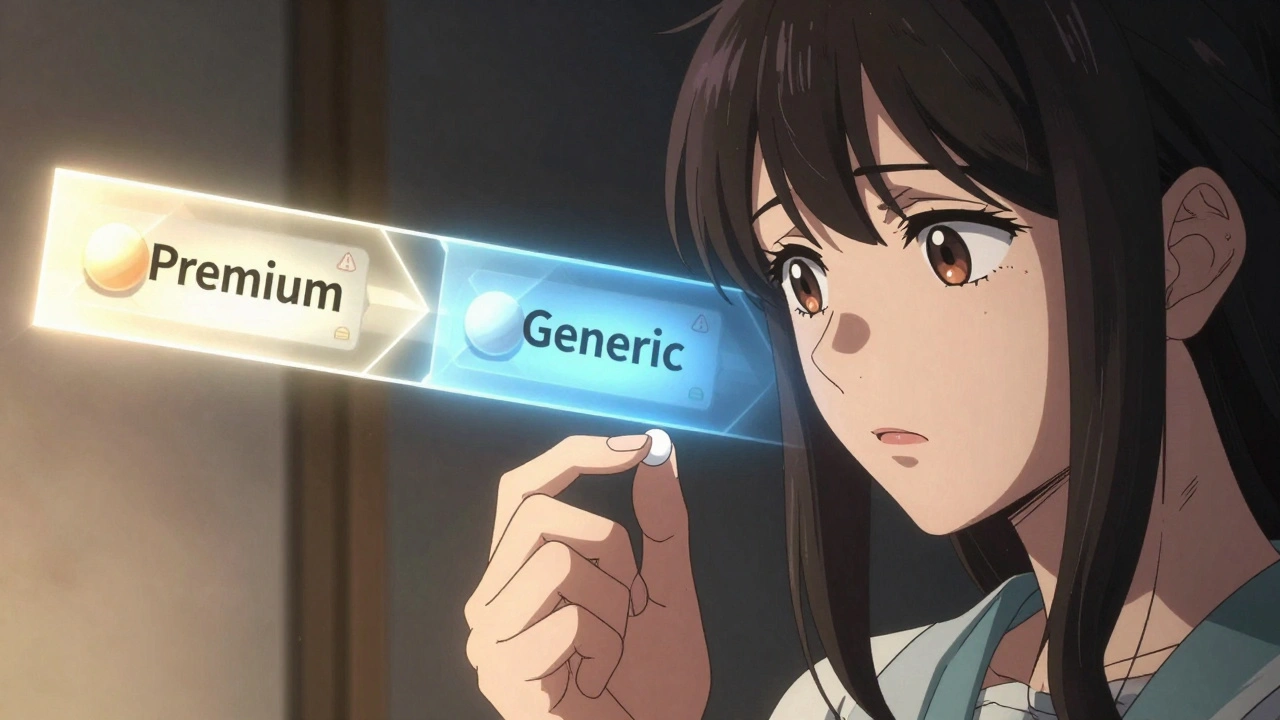
Labeling Effect: How Generic Drug Labels Influence Your Body’s Response
Dec 2, 2025, Posted by Mike Clayton
Generic drugs are chemically identical to brand-name versions, but many patients believe they’re less effective. This psychological bias-called the labeling effect-can reduce adherence, worsen symptoms, and cost the healthcare system billions. Here’s how the label changes your body’s response.
MORESEARCH HERE
Categories
TAGS
- treatment
- online pharmacy
- dietary supplement
- side effects
- generic drugs
- medication adherence
- medication safety
- health
- dietary supplements
- health benefits
- online pharmacy Australia
- generic substitution
- adverse drug reactions
- thyroid disorders
- gabapentin
- treatment option
- calcipotriol
- blood pressure
- erectile dysfunction
- closer look
