Geriatric Pharmacotherapy: Safe Medication Use for Older Adults
When we talk about geriatric pharmacotherapy, the specialized approach to prescribing and managing medications for older adults. Also known as age-appropriate drug therapy, it’s not just about giving the right pill—it’s about understanding how aging changes how the body handles drugs, how multiple conditions interact, and why what works for a 40-year-old can harm an 80-year-old. Your kidneys slow down. Your liver processes drugs differently. Your brain becomes more sensitive to sedatives. These aren’t minor tweaks—they’re major shifts that turn common prescriptions into hidden risks.
That’s why polypharmacy, the use of five or more medications at once. Also known as multiple drug regimens, it’s so common in older adults that nearly half take eight or more pills daily. But more pills don’t mean better health. They mean more chances for dangerous drug interactions, when one medication changes how another works in the body. Also known as medication conflicts, these can cause falls, confusion, bleeding, or kidney failure. Warfarin and antibiotics? A risky mix. Cranberry juice and blood thinners? Can spike INR levels. Even common painkillers like ibuprofen can wreck kidney function in someone with reduced renal clearance. These aren’t edge cases—they’re daily realities in clinics treating seniors.
And then there’s renal impairment in elderly, the gradual decline in kidney function that affects up to 50% of adults over 70. Also known as age-related kidney changes, it means drugs like metformin, statins, or antibiotics stay in the body longer, building up to toxic levels. Doctors don’t always adjust doses because they’re not trained to check creatinine clearance properly—or they assume "normal" lab ranges apply to everyone. But a creatinine level that looks fine for a 30-year-old could mean severe kidney trouble in someone 85. That’s why bringing your actual pill bottles to appointments isn’t just smart—it’s life-saving. It’s the only way to catch hidden duplicates, outdated prescriptions, or dangerous combinations your doctor might miss.
What you’ll find in these posts isn’t theory. It’s real-world guidance from people who’ve seen the fallout: the elderly patient who developed delirium from a simple antibiotic, the senior who stopped statins because of muscle pain and didn’t know how to do it safely, the caregiver who didn’t realize cranberry juice was raising their parent’s bleeding risk. These aren’t rare stories. They’re the quiet emergencies happening in living rooms across the country. This collection gives you the tools to spot them before they happen—and the knowledge to ask the right questions when a doctor says, "This is fine."
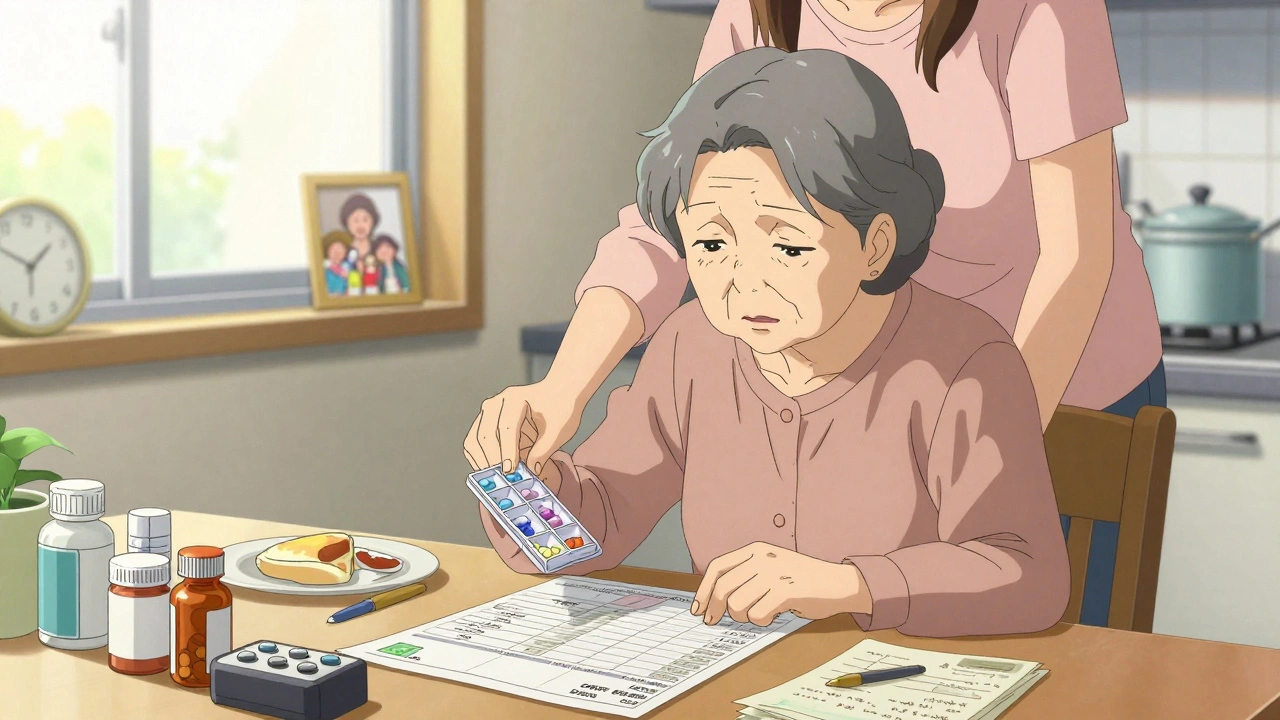
How to Simplify Complex Medication Regimens for Older Adults
Dec 9, 2025, Posted by Mike Clayton
Simplify complex medication regimens for older adults by reducing pill burden, combining doses, and aligning schedules with daily life. Proven strategies improve adherence, safety, and independence without compromising care.
MORESEARCH HERE
Categories
TAGS
- treatment
- online pharmacy
- dietary supplement
- side effects
- generic drugs
- medication adherence
- medication safety
- health
- dietary supplements
- health benefits
- online pharmacy Australia
- generic substitution
- adverse drug reactions
- thyroid disorders
- gabapentin
- treatment option
- calcipotriol
- blood pressure
- erectile dysfunction
- closer look
