When a woman’s body doesn’t produce enough natural progesterone, it can lead to irregular periods, difficulty getting pregnant, or early miscarriages. That’s where dydrogesterone comes in. Unlike synthetic hormones that mimic other steroids, dydrogesterone is designed to act almost exactly like the body’s own progesterone. It doesn’t mess with other hormone systems. It doesn’t cause unwanted side effects like weight gain or mood swings in most people. It simply does one thing very well: supports the lining of the uterus so pregnancy can happen and be maintained.
What Makes Dydrogesterone Different from Other Progestins?
Not all progesterone-like drugs are the same. Many older progestins were created by tweaking testosterone or other male hormones. That’s why they sometimes cause acne, hair growth, or voice changes - side effects tied to androgenic activity. Dydrogesterone is different. It was developed in the 1960s specifically to avoid those problems. Its chemical structure is nearly identical to natural progesterone, just with one small twist: a double bond between carbons 6 and 7. That tiny change makes it resistant to being broken down too quickly by the liver, so it lasts longer in the body without needing high doses.
Because of this, dydrogesterone binds tightly to progesterone receptors in the uterus, ovaries, and brain - but barely touches receptors for testosterone, estrogen, or cortisol. This precision is why doctors choose it for fertility treatments, recurrent miscarriage, and luteal phase defects. It’s not a general hormone blast. It’s a targeted tool.
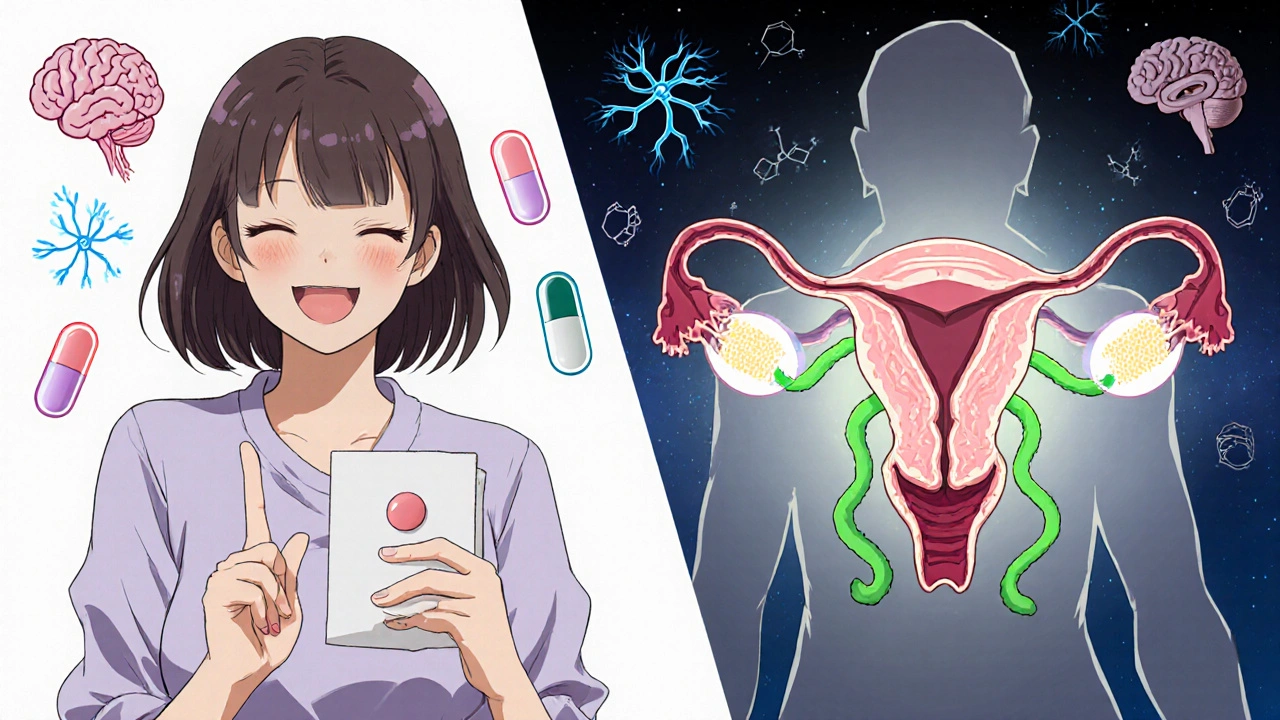
How Dydrogesterone Affects the Uterus
The key job of progesterone - whether natural or synthetic - is to prepare the endometrium, the inner lining of the uterus, for a fertilized egg. After ovulation, your body normally ramps up progesterone. If pregnancy doesn’t happen, that level drops, and you get your period. If it does, progesterone stays high to keep the lining thick, soft, and full of blood vessels so the embryo can implant and grow.
Dydrogesterone steps in when the body doesn’t make enough progesterone on its own. It attaches to progesterone receptors in the endometrial cells. Once bound, it triggers a chain reaction: genes turn on that produce proteins needed for implantation. Blood vessels grow. Mucus thickens to protect the embryo. The immune system in the uterus shifts to tolerate the foreign tissue (the embryo) instead of attacking it.
Studies show that dydrogesterone increases the thickness of the endometrium by 20-30% in women with luteal phase deficiency. In one trial of 400 women with recurrent miscarriage, those taking dydrogesterone had a 75% success rate in carrying to term, compared to 52% in the placebo group. That’s not magic. That’s biology.
Its Role in the Brain and Ovaries
Dydrogesterone doesn’t just work in the uterus. It also crosses the blood-brain barrier and acts on the hypothalamus and pituitary gland. Here’s where it gets clever: it doesn’t suppress ovulation like birth control pills do. Instead, it gently modulates the feedback loop that controls LH (luteinizing hormone) and FSH (follicle-stimulating hormone).
In women undergoing fertility treatments, this means dydrogesterone helps maintain the luteal phase - the second half of the cycle - without interfering with ovulation. That’s critical. You don’t want to stop ovulation if you’re trying to get pregnant. You want to support what’s already happened. Dydrogesterone does that. It doesn’t block the natural hormone surge. It just makes sure the aftermath is strong enough to hold onto a pregnancy.
It also helps regulate the corpus luteum, the temporary gland that forms after ovulation and normally produces progesterone. If that gland doesn’t last long enough or doesn’t produce enough, dydrogesterone fills the gap. Think of it like a backup battery for your body’s natural system.
Why It Doesn’t Cause the Side Effects of Other Hormones
Many women worry about hormone therapy because of bad experiences with older drugs. They’ve heard stories about blood clots, depression, or bloating. Dydrogesterone has a clean safety profile because it doesn’t interact with other hormone pathways.
It doesn’t increase SHBG (sex hormone-binding globulin), which means it doesn’t lower free testosterone levels - so no loss of libido. It doesn’t affect liver enzymes the way some oral progestins do, so it doesn’t raise triglycerides or increase clotting risk. It doesn’t bind to mineralocorticoid receptors, so no water retention or high blood pressure.
In clinical trials, the most common side effects were mild: occasional headache, breast tenderness, or slight nausea - and those happened in fewer than 5% of users. Compare that to medroxyprogesterone, where up to 30% report mood changes or weight gain. Dydrogesterone’s selectivity is its biggest advantage.
When Is It Used? Real-World Scenarios
Dydrogesterone isn’t for everyone. But for specific cases, it’s often the first choice:
- Women with luteal phase defect - where progesterone stays too low for too long after ovulation.
- Those undergoing IVF or other assisted reproductive technologies - to support the uterine lining after embryo transfer.
- Women who’ve had two or more unexplained miscarriages - especially if progesterone levels were low in early pregnancy.
- Women with irregular cycles due to anovulation - to induce a regular withdrawal bleed and reset the cycle.
- Those with endometriosis - as part of long-term hormonal management to suppress growth of endometrial tissue outside the uterus.
It’s usually taken orally, once or twice daily, starting right after ovulation and continuing until the 10th to 12th week of pregnancy if conception occurs. Some doctors stop it earlier, others keep it going longer. There’s no one-size-fits-all, but the goal is always the same: keep progesterone levels stable until the placenta takes over.
How Long Does It Take to Work?
Dydrogesterone starts binding to receptors within 30 minutes of taking a pill. But biological effects take longer. The endometrial thickening you see on an ultrasound usually appears after 7-10 days of consistent use. That’s why doctors don’t expect immediate results. You need at least one full cycle to see if it’s working.
For women trying to conceive, doctors often recommend taking it for three cycles before evaluating success. If pregnancy doesn’t happen after that, they look for other causes - like thyroid issues, blocked tubes, or sperm quality. Dydrogesterone fixes one problem: low progesterone. It doesn’t fix everything.
What Happens When You Stop Taking It?
If you’re taking dydrogesterone to regulate your cycle and you stop, you’ll usually get a withdrawal bleed within 3-7 days. That’s normal. It’s not a period - it’s the lining shedding because the hormone support is gone.
If you’re pregnant and stop suddenly, you might worry about miscarriage. But studies show that once the placenta starts producing progesterone (around week 8-10), the body doesn’t need external support anymore. Stopping dydrogesterone at that point doesn’t increase miscarriage risk. In fact, continuing beyond 12 weeks is unnecessary and not recommended.
The key is tapering only if advised by your doctor. Abruptly stopping during early pregnancy without medical guidance isn’t safe - but that’s true for any hormone therapy.
Common Myths About Dydrogesterone
- Myth: It causes birth defects. Fact: Over 50 years of use and dozens of studies show no increased risk of congenital abnormalities. It’s classified as Category A in pregnancy safety by the FDA - meaning no evidence of harm in human studies.
- Myth: It’s the same as progesterone injections. Fact: Injections deliver high peaks and low troughs. Dydrogesterone gives steady, consistent levels through the gut. That’s why it’s better tolerated.
- Myth: You need to take it forever. Fact: Most courses last 3-6 months. For recurrent miscarriage, it’s usually only needed during early pregnancy, not long-term.
Dydrogesterone isn’t a miracle drug. But when progesterone deficiency is the issue, it’s one of the most reliable, safest, and best-studied options available. It doesn’t overpromise. It doesn’t overdo it. It just does its job - quietly, precisely, and effectively.
Can dydrogesterone help me get pregnant if I have PCOS?
Dydrogesterone won’t fix the root cause of PCOS - like insulin resistance or high androgens. But if you’re not ovulating regularly or have a short luteal phase because of PCOS, it can help support the uterine lining after ovulation. Many women with PCOS take clomiphene or letrozole to trigger ovulation, then add dydrogesterone to improve implantation chances. It’s not a standalone solution, but it’s often part of the plan.
Is dydrogesterone safe during breastfeeding?
Dydrogesterone passes into breast milk in very small amounts, and no adverse effects have been reported in nursing infants. However, because it’s a hormone, most doctors avoid prescribing it while breastfeeding unless absolutely necessary. Natural progesterone levels drop after birth to allow milk production, and adding synthetic progesterone might interfere with that. Always talk to your doctor before using it while nursing.
Does dydrogesterone cause weight gain?
Unlike some older progestins, dydrogesterone doesn’t cause water retention or increase appetite. Weight gain isn’t a common side effect. Some women report slight bloating early on, but that usually goes away. If you notice unexplained weight gain, it’s more likely due to diet, stress, or another condition - not dydrogesterone.
How does dydrogesterone compare to natural progesterone creams?
Natural progesterone creams are marketed as "bio-identical," but they’re poorly absorbed through the skin. Studies show they rarely raise blood progesterone levels enough to be effective for pregnancy support. Dydrogesterone, taken orally, delivers consistent, measurable levels in the bloodstream. It’s FDA-approved and backed by clinical trials. Creams are not.
Can I take dydrogesterone with other fertility drugs?
Yes. It’s commonly combined with clomiphene, letrozole, or gonadotropins. It’s also used after embryo transfer in IVF cycles. There are no dangerous interactions. But timing matters. Dydrogesterone is usually started after ovulation or embryo transfer - never before. Taking it too early can interfere with follicle development. Always follow your doctor’s schedule.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.