When your thyroid-stimulating hormone (TSH) is high but your free T4 is normal, you have subclinical hypothyroidism. It’s not the same as full-blown hypothyroidism. You might not feel sick. Your doctor might say, "Wait and watch." But should you? Or should you start levothyroxine right away? The answer isn’t simple. It depends on your age, your antibodies, your symptoms, and even which lab did your blood test.
What Exactly Is Subclinical Hypothyroidism?
Subclinical hypothyroidism means your pituitary gland is working overtime to tell your thyroid to produce more hormone. Your TSH is up-usually above 4.0 mIU/L-but your free T4, the active thyroid hormone, is still in the normal range. That’s why it’s called "subclinical"-there’s no clear clinical sign yet. But that doesn’t mean nothing’s happening.
This isn’t rare. About 1 in 5 adults in the U.S. have elevated TSH without low T4. The numbers climb with age. In people over 60, it’s more common than high blood pressure. But not everyone with elevated TSH needs treatment. In fact, many don’t.
When Is TSH Really Too High?
Here’s where things get messy. Labs don’t all agree on what "normal" TSH is. Some say up to 4.5 mIU/L is fine. Others use 5.0. A few now use age-adjusted ranges-like 2.5 for people under 50. That’s important because if your lab uses 4.5 as the upper limit, and yours is 4.8, you’re flagged. But if your lab uses 5.0, you’re fine. That’s not a medical change-it’s a lab change.
The real debate starts at TSH levels between 4.0 and 10.0 mIU/L. Below 4.0? Usually not a problem. Above 10.0? Most experts agree you should treat. But what about that gray zone? That’s where the confusion lives.
What Does the Evidence Say?
Let’s look at the data. A big study in JAMA in 2017 followed 737 older adults with TSH between 4 and 10. They gave half levothyroxine. The other half got nothing. After a year, there was no difference in energy, mood, memory, or quality of life. The treatment didn’t help.
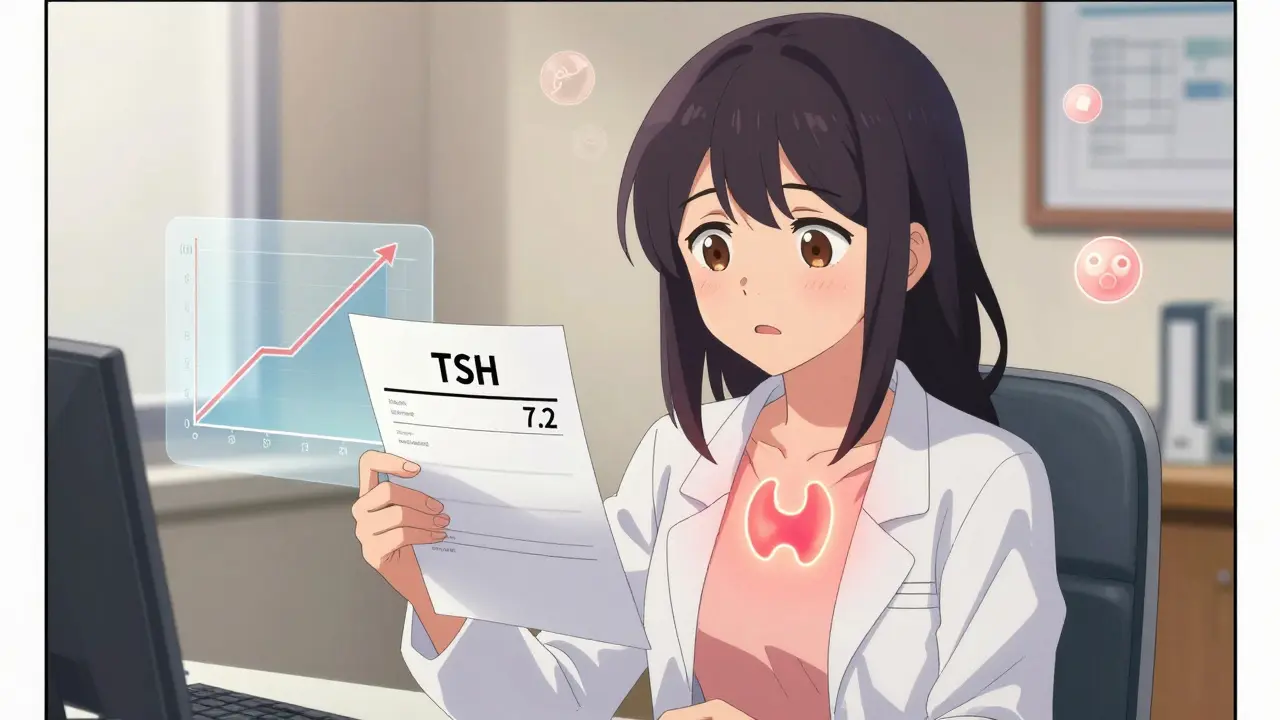
But that’s not the whole story. Another study in 2020 looked at people under 50 with TSH between 7 and 10 and positive thyroid antibodies. In that group, 32% reported fewer symptoms like fatigue and brain fog after starting low-dose levothyroxine. That’s a real benefit for someone struggling every day.
Then there’s the progression risk. If your TSH is above 8 mIU/L and you have thyroid antibodies (TPOAb), you have a 70% chance of developing full hypothyroidism within four years. That’s not a small risk. It means your thyroid is slowly failing. And once it fails, you’ll need lifelong medication anyway. Starting early might just delay the inevitable.
Thyroid Antibodies Change Everything
This is one of the most overlooked factors. If you test positive for thyroid peroxidase antibodies (TPOAb), your immune system is attacking your thyroid. That’s Hashimoto’s-even if you don’t have symptoms yet. Antibody-positive patients are far more likely to progress. Studies show they’re 2.3 times more likely to develop overt hypothyroidism than those without antibodies.
So if your TSH is 6.5 and your antibodies are high? Treatment is much more likely to help. If your TSH is 8.2 and antibodies are negative? You might never progress. Monitoring is the smarter move.
Age Matters More Than You Think
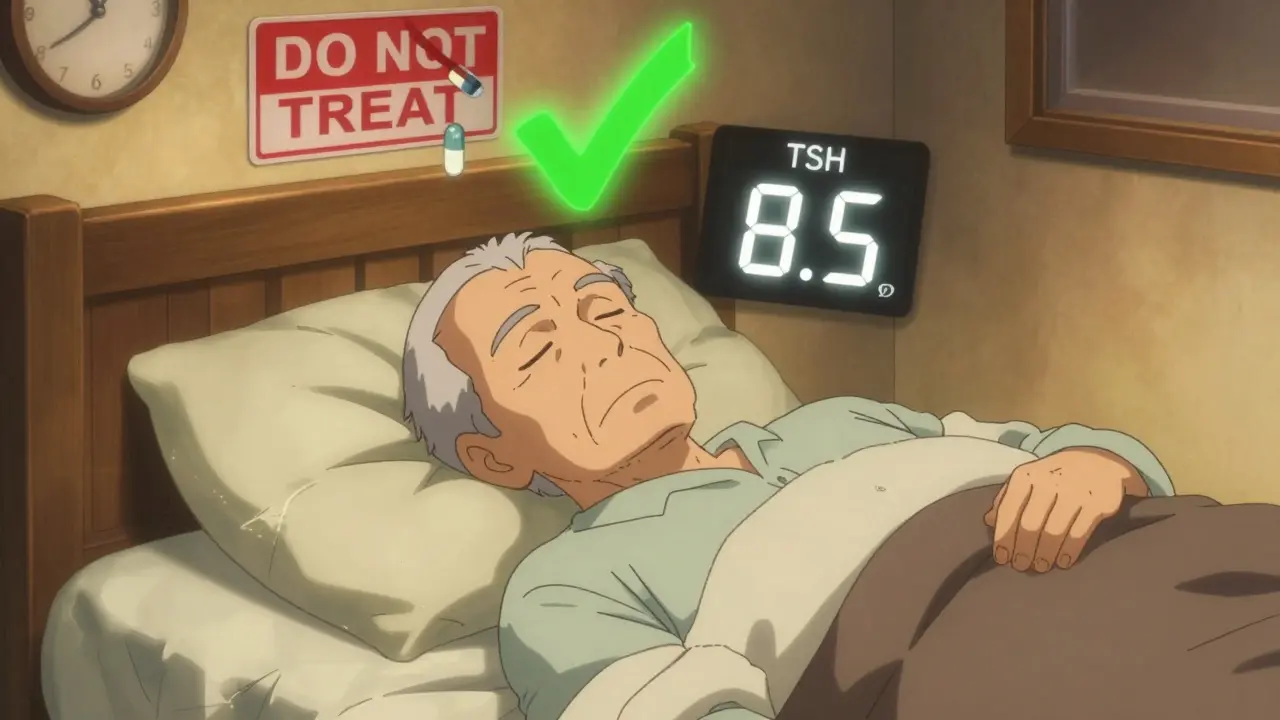
For people over 65, treating subclinical hypothyroidism can be dangerous. A 2021 meta-analysis found that treating TSH levels under 10 in older adults led to a 12.3% higher risk of death. Why? Because levothyroxine can overstimulate the heart. It can cause atrial fibrillation, bone loss, and muscle weakness in older people.
That’s why major guidelines from the American Academy of Family Physicians and the Royal Australian College of General Practitioners say: don’t treat anyone over 65 with TSH under 10. Let it be. Monitor every 6 to 12 months. Don’t rush to medication.
But for someone in their 30s or 40s? The story flips. If they have symptoms, antibodies, and TSH above 7, treatment might prevent future problems. It’s not about fixing a problem today-it’s about stopping one from getting worse.
Do Symptoms Even Matter?
People with subclinical hypothyroidism often report fatigue, weight gain, dry skin, or brain fog. But here’s the catch: those same symptoms show up in healthy people too. Studies found that 30-40% of people with normal thyroid function report "hypothyroid symptoms." So how do you know if your fatigue is from your thyroid-or from too much coffee, poor sleep, or stress?
That’s why doctors now use tools like the Thyroid-Related Quality of Life Patient-Reported Outcome (ThyPRO) questionnaire. It’s not a guess. It’s a score. If your score is high and your TSH is over 7 with positive antibodies, treatment becomes more justifiable. If your score is low? You’re probably fine without pills.
When Should You Start Treatment?
Based on the evidence, here’s a practical guide:
- TSH over 10 mIU/L: Treat. Most guidelines agree. The risk of progression is high. The benefit of treatment is clear.
- TSH 7-10 mIU/L with positive TPO antibodies: Consider treatment, especially if you’re under 50. You’re at high risk of progression. Symptom relief is possible.
- TSH 7-10 mIU/L with negative antibodies: Monitor. Don’t treat. Progression risk is low. Treatment won’t likely help.
- TSH 4-7 mIU/L: Don’t treat. No evidence of benefit. Only monitor if you’re pregnant or planning pregnancy.
- Over age 65: Don’t treat unless TSH is over 10 and you have clear symptoms. Avoid medication if possible.
Start with a low dose: 25-50 mcg of levothyroxine daily. Recheck TSH in 6-8 weeks. Adjust slowly. The goal isn’t to get TSH to zero. It’s to bring it into the normal range without overdoing it.

What You Should Do Next
If you’ve been told your TSH is high but your T4 is normal, here’s what to ask your doctor:
- "What’s my exact TSH number? Which lab’s reference range are we using?"
- "Have I been tested for thyroid antibodies (TPOAb)?"
- "Am I under 50? Over 65?"
- "Do I have symptoms that match thyroid dysfunction?"
- "What’s my cardiovascular risk? Do I have high cholesterol or heart rhythm issues?"
Don’t rush into medication. Don’t ignore it either. Get the full picture. One blood test doesn’t tell the whole story. Two tests, six weeks apart, are the minimum. Antibody testing is non-negotiable if you’re in the gray zone.
What About Natural Fixes?
Some people turn to selenium, iodine, or gluten-free diets. But here’s the truth: there’s no solid evidence that diet changes reverse subclinical hypothyroidism. Selenium might lower antibodies slightly in Hashimoto’s, but it doesn’t prevent progression. Iodine? Only help if you’re deficient-and most people aren’t. Gluten-free diets? Only help if you have celiac disease. Otherwise, they won’t fix your TSH.
Medication isn’t perfect. But for the right person, it’s the only thing that reliably brings TSH down and stops the thyroid from failing. Natural fixes are distractions. Don’t waste time on them while your thyroid slowly declines.
What’s Coming Next?
Researchers are now looking at TSH velocity-how fast your TSH is rising over time. If your TSH jumps by more than 1 mIU/L per month, your risk of progression shoots up. New tools from companies like Roche Diagnostics can now track this trend automatically using past lab results.
Also, the 2023 American Thyroid Association draft guidelines may soon recommend treating people under 30 with TSH over 7 and positive antibodies. That’s a shift toward earlier action in younger, high-risk groups.
For now, stick to the evidence. Don’t treat based on fear. Don’t ignore based on convenience. Use your numbers, your age, your antibodies, and your symptoms to make a smart choice.
Is subclinical hypothyroidism the same as Hashimoto’s?
No. Subclinical hypothyroidism is a lab finding-elevated TSH with normal T4. Hashimoto’s is an autoimmune disease where the immune system attacks the thyroid. Many people with subclinical hypothyroidism have Hashimoto’s (especially if TPO antibodies are positive), but not all do. You can have subclinical hypothyroidism without Hashimoto’s if your antibodies are negative.
Can subclinical hypothyroidism go away on its own?
Yes, sometimes. About 20-30% of people with mild TSH elevation (4-7 mIU/L) and negative antibodies return to normal within a year without treatment. That’s why monitoring is key. If your TSH drops back into range, you don’t need medication. But if it keeps climbing, especially above 8 mIU/L, treatment becomes more likely.
Why do some doctors treat TSH 5-6 and others wait until 10?
It’s a mix of guidelines, training, and experience. Endocrinologists often see patients who’ve progressed to full hypothyroidism and want to prevent that. Primary care doctors see more elderly patients where treatment carries risks. The American Thyroid Association says wait until 10. The American Association of Clinical Endocrinologists says consider treatment at 7. Both are based on real data-but different priorities.
Does treating subclinical hypothyroidism lower cholesterol?
In some cases, yes. Studies show levothyroxine can lower LDL (bad) cholesterol by 8-12% in patients with TSH over 7 and positive antibodies. But this benefit is small and only seen in younger patients. For older adults, the heart risks outweigh this small gain. It’s not a reason to treat everyone.
How often should I get my TSH checked if I’m not being treated?
If your TSH is between 4 and 10 and you’re not on medication, check it every 6 to 12 months. If it’s stable, you can stretch to every year. If it’s rising quickly-say, jumping from 5 to 7 in 6 months-check every 3-6 months. Don’t wait years. Thyroid function can change faster than you think.

Author
Mike Clayton
As a pharmaceutical expert, I am passionate about researching and developing new medications to improve people's lives. With my extensive knowledge in the field, I enjoy writing articles and sharing insights on various diseases and their treatments. My goal is to educate the public on the importance of understanding the medications they take and how they can contribute to their overall well-being. I am constantly striving to stay up-to-date with the latest advancements in pharmaceuticals and share that knowledge with others. Through my writing, I hope to bridge the gap between science and the general public, making complex topics more accessible and easy to understand.