Exudative Effusion: Causes, Risks, and How Medications Affect Fluid Buildup
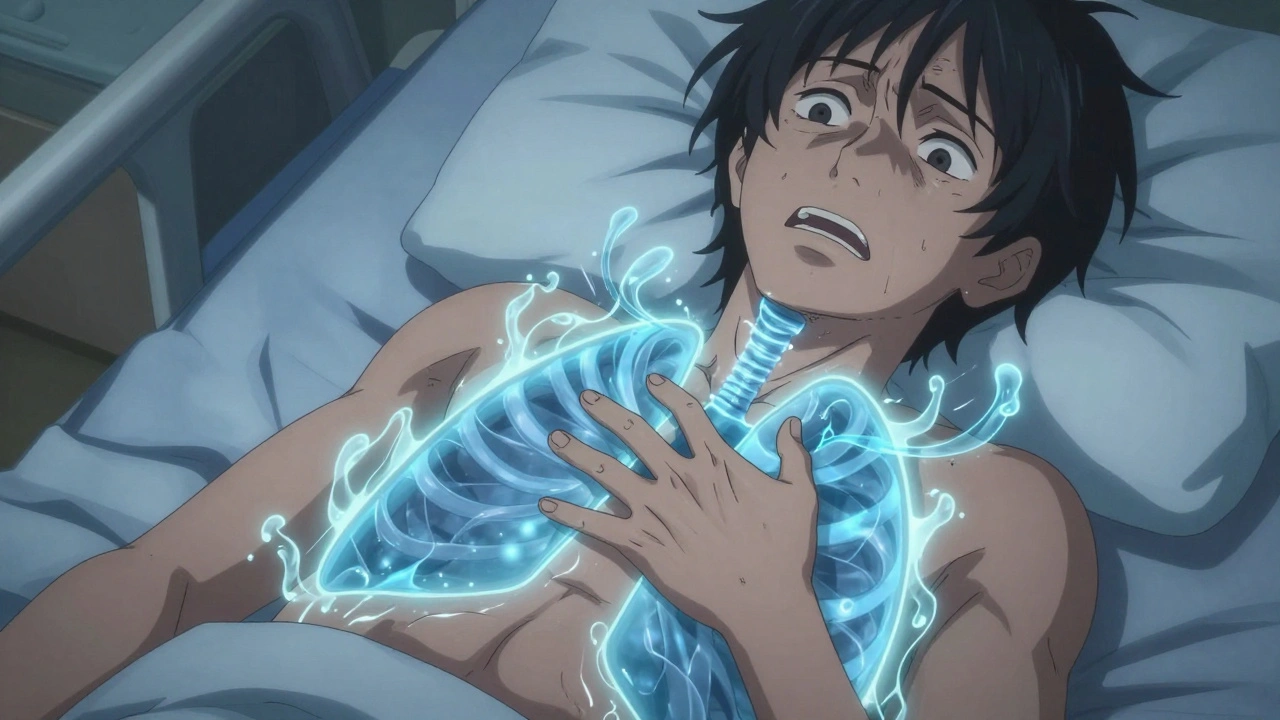
When your body’s natural filters break down, exudative effusion, a type of fluid buildup caused by inflammation, infection, or injury that leaks protein-rich fluid into body cavities. Also known as inflammatory effusion, it’s not just water pooling—it’s a sign something deeper is wrong. Unlike transudative effusions, which come from pressure changes like heart failure, exudative effusions are driven by damaged blood vessels. Think of it like a leaky pipe under pressure—only here, the pipe is your capillary, and the pressure is inflammation.
This kind of fluid buildup most often shows up in the pleural space, the area around the lungs where excess fluid can make breathing hard, but it can also happen in the abdomen (ascites) or around the heart (pericardial effusion). What makes it dangerous isn’t just the fluid—it’s what’s in it. High protein, lots of white blood cells, sometimes even bacteria or cancer cells. That’s why doctors don’t just drain it and call it done. They test it. They look for infections like pneumonia, autoimmune diseases like lupus, or tumors. And they check if your meds might be making it worse. For example, drugs like minocycline, an antibiotic sometimes linked to drug-induced lupus, or even long-term use of certain NSAIDs, common painkillers that can trigger kidney issues and fluid retention, have been tied to exudative reactions.
It’s not just about what you’re taking—it’s about what’s already wrong inside you. If you have kidney disease, your body struggles to flush out extra fluid. If you have heart failure, you might get transudative fluid—but if infection hits on top of that, it can turn into exudative. That’s why drug-disease interactions, when a medication for one condition worsens another, matter so much here. A drug meant to lower blood pressure might accidentally make fluid buildup worse in someone with liver cirrhosis. Or an antibiotic meant to treat pneumonia could trigger an allergic reaction that turns into a leaky pleural space.
You’ll find posts here that dig into how medications affect fluid balance—from how antibiotics can trigger immune responses leading to effusion, to how diuretics might not work the same if your kidneys are already damaged. You’ll see how drug interactions with conditions like diabetes or autoimmune disorders can quietly worsen inflammation. And you’ll learn how to spot the early signs: unexplained shortness of breath, swelling in the belly, sudden weight gain, or chest pain that doesn’t go away with rest.
This isn’t just medical jargon. It’s about knowing when your body is screaming for help—and what to do before it gets worse. Whether you’re managing a chronic illness, taking multiple meds, or just wondering why you’re feeling off, the posts below give you real, practical answers. No fluff. Just what you need to understand what’s happening inside you, and how to talk to your doctor about it.
Pleural Effusion: Understanding Causes, Thoracentesis, and How to Prevent Recurrence
Dec 3, 2025, Posted by Mike Clayton
Pleural effusion is fluid buildup around the lungs, often caused by heart failure, pneumonia, or cancer. Learn how thoracentesis works, what tests are done, and how to stop it from coming back.
MORESEARCH HERE
Categories
TAGS
- treatment
- online pharmacy
- dietary supplement
- side effects
- generic drugs
- medication adherence
- medication safety
- health
- dietary supplements
- health benefits
- online pharmacy Australia
- generic substitution
- adverse drug reactions
- thyroid disorders
- gabapentin
- treatment option
- calcipotriol
- blood pressure
- erectile dysfunction
- closer look
