Hydration for Diabetics: Why Water Matters and What to Avoid
When you have diabetes, hydration for diabetics, the practice of maintaining adequate fluid intake to support blood sugar balance and kidney function. It’s not just about drinking water—it’s about managing how your body handles fluids when insulin isn’t working right. High blood sugar pulls water out of your cells, making you thirsty and urinating more. If you don’t replace that lost fluid, you risk dehydration, which can spike your blood sugar even higher. It’s a cycle: high sugar → more urination → less water → higher sugar. Breaking it starts with understanding how water affects your body.
blood sugar control, the process of keeping glucose levels within a safe range through diet, medication, and fluid intake depends heavily on hydration. When you’re dehydrated, your kidneys hold onto sugar instead of flushing it out. That means your blood sugar stays elevated longer. Studies show that even mild dehydration can raise HbA1c levels over time. And if you’re taking medications like SGLT2 inhibitors—drugs that make you pee out extra sugar—you’re at even higher risk. That’s why drinking water isn’t optional; it’s part of your treatment plan.
dehydration in diabetes, a dangerous condition where fluid loss outpaces intake, often leading to dizziness, confusion, or even diabetic ketoacidosis doesn’t always feel like thirst. Older adults, especially those with type 2 diabetes, may not feel thirsty even when they’re dangerously low on fluids. Signs include dry mouth, dark urine, fatigue, and confusion. If you’re sick, exercising, or in hot weather, you need more water—not less. Skip sugary drinks, energy drinks, and fruit juices. They raise blood sugar fast and make dehydration worse. Even diet sodas can mess with your gut and make you crave more sugar.
electrolyte balance, the regulation of minerals like sodium, potassium, and magnesium that help nerves and muscles work properly matters too. When you lose water through frequent urination, you lose electrolytes. That’s why plain water isn’t always enough—especially during illness or intense heat. But don’t reach for sports drinks. Most are loaded with sugar. Instead, try sugar-free electrolyte tablets or homemade solutions with a pinch of salt and a splash of lemon. Talk to your doctor before using any supplements.
diabetic fluid intake, the daily amount and type of liquids consumed to support health without spiking glucose should be consistent and smart. Aim for at least 8 cups a day, more if you’re active or it’s hot. Track how much you drink. Set reminders. Keep a bottle handy. Avoid alcohol—it dehydrates you and can mask low blood sugar symptoms. Herbal teas and black coffee (without sugar or cream) count toward your total. The goal isn’t to drink until you’re bloated—it’s to drink enough to keep your urine light yellow and your body running smoothly.
What you’ll find below are real, practical guides on how hydration connects to your meds, your diet, and your daily risks. From what to drink when you’re on metformin, to why cranberry juice isn’t always safe, to how contrast dye affects your kidneys—these posts give you the facts without the fluff. No guesses. No myths. Just what works.
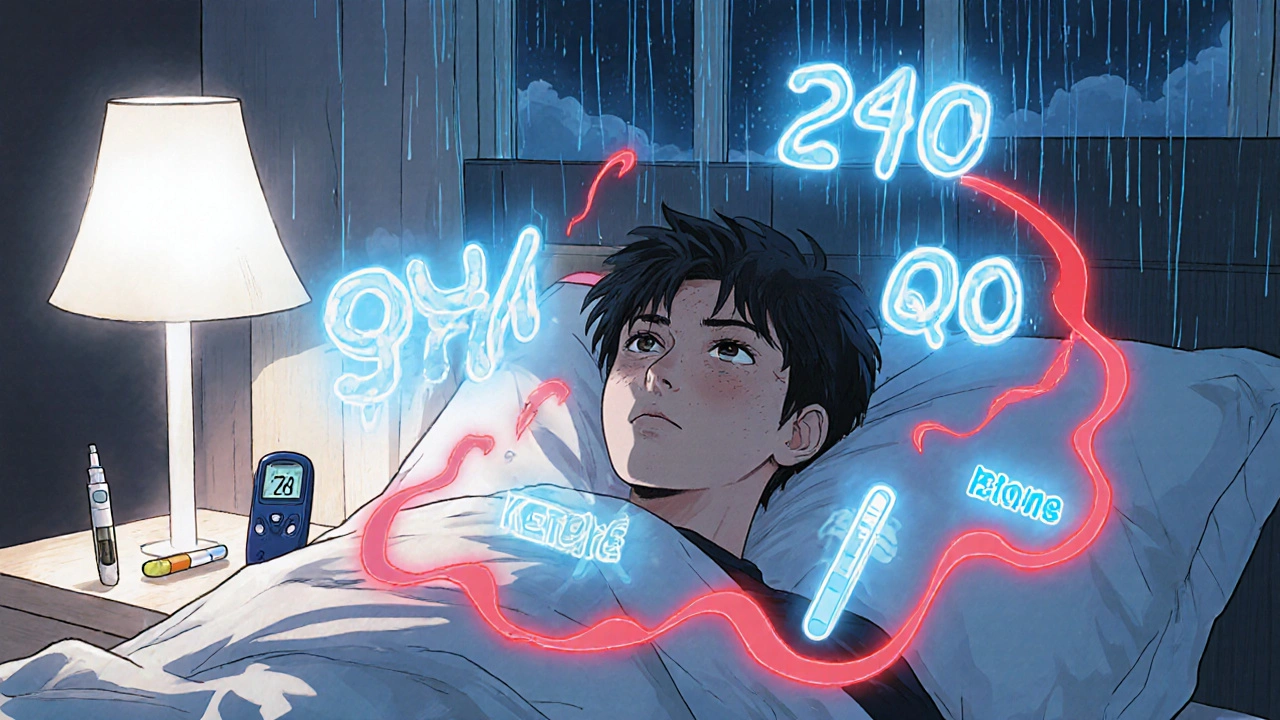
Sick Day Rules for Diabetes: Insulin, Hydration, and Ketone Checks
Nov 22, 2025, Posted by Mike Clayton
Learn the essential sick day rules for diabetes: never skip insulin, check blood sugar every few hours, stay hydrated with the right fluids, and test for ketones to prevent dangerous complications like diabetic ketoacidosis.
MORESEARCH HERE
Categories
TAGS
- treatment
- online pharmacy
- dietary supplement
- side effects
- generic drugs
- medication adherence
- medication safety
- health
- dietary supplements
- health benefits
- online pharmacy Australia
- generic substitution
- adverse drug reactions
- thyroid disorders
- gabapentin
- treatment option
- calcipotriol
- blood pressure
- erectile dysfunction
- closer look
