Insulin During Illness: What You Need to Know About Dosing and Safety
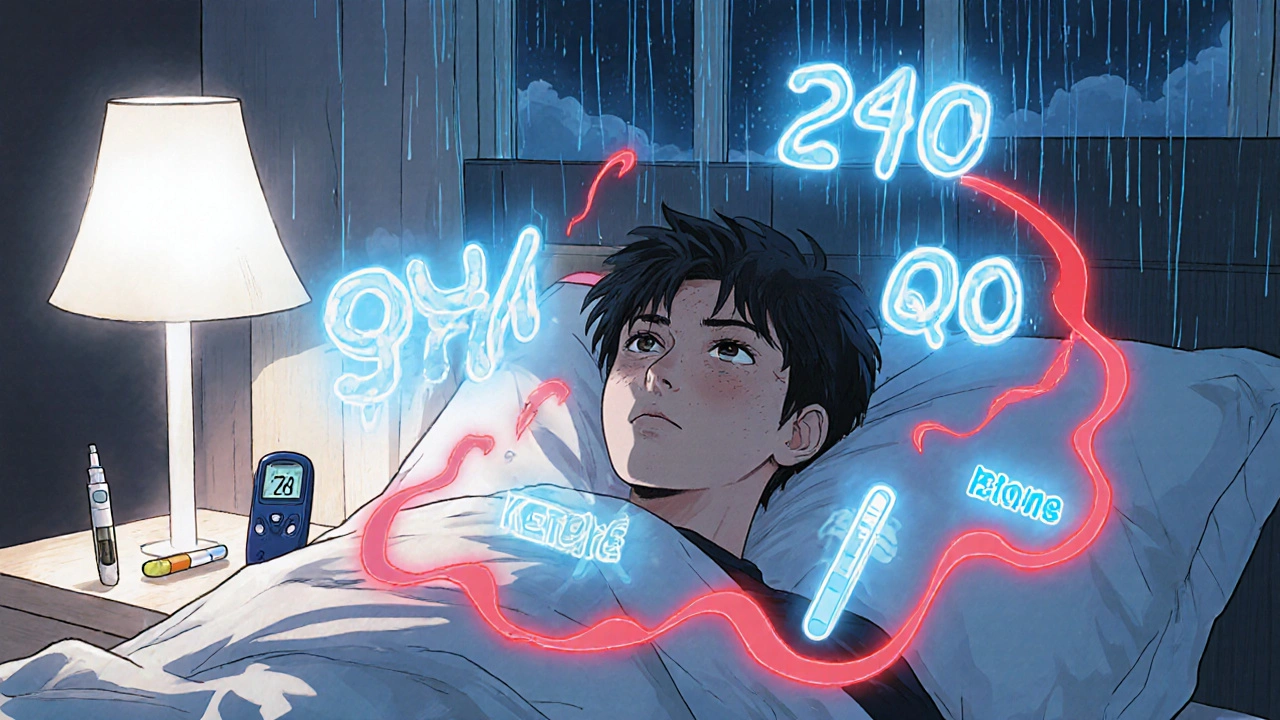
When you have diabetes, getting sick doesn’t just mean feeling bad—it can throw your insulin during illness, the way your body uses insulin when you’re unwell, often requiring different dosing than when you’re healthy. Also known as sick-day insulin management, this isn’t optional. Skipping insulin or guessing doses can lead to dangerous spikes, dehydration, or even diabetic ketoacidosis. Your body releases stress hormones like cortisol and adrenaline when you’re sick, and those hormones fight insulin. That means even if you’re not eating, your blood sugar can still rise—and fast.
This is why blood sugar control, the practice of keeping glucose levels within a safe range, especially during physical stress becomes critical. You don’t need to eat to need insulin. Your liver keeps pumping out glucose, and without enough insulin, your body starts breaking down fat for energy, producing toxic ketones. That’s how diabetic ketoacidosis starts. People with type 1 diabetes are at highest risk, but type 2 patients on insulin can also get sick enough to need urgent care. Monitoring your blood sugar every 2 to 4 hours isn’t overkill—it’s survival.
insulin adjustment, the process of changing your insulin dose based on illness, food intake, and blood sugar trends isn’t about being perfect. It’s about being proactive. If your blood sugar is over 240 mg/dL, check for ketones. If you’re vomiting or can’t keep fluids down, don’t wait. Call your doctor. Most people need to keep taking their basal insulin—even if they’re not eating—and may need extra rapid-acting insulin to correct highs. Some might need to switch to a different insulin type temporarily. No two illnesses are the same. A cold might need a small tweak. The flu or pneumonia? That’s a full emergency plan.
You also need to think about diabetic ketoacidosis, a life-threatening condition caused by severe insulin shortage during illness, leading to high blood sugar and dangerous acid buildup. Symptoms? Excessive thirst, frequent urination, nausea, confusion, fruity-smelling breath, and trouble breathing. If you see these, don’t wait for your next appointment. Go to the ER. This isn’t something you can treat with a home remedy. Hospitals have IV fluids and insulin drips for a reason.
Keep a sick-day plan ready. Write down your doctor’s instructions for insulin changes, when to test ketones, what fluids to drink, and who to call. Keep glucose tablets or juice on hand—not to treat lows, but to prevent them if you’re not eating. Don’t stop insulin just because you’re not hungry. And don’t rely on over-the-counter meds that might raise blood sugar, like some cough syrups. Always check labels.
Below, you’ll find real, practical advice from people who’ve been through this—how they adjusted insulin during infections, what mistakes they made, and how they learned to stay safe. These aren’t theory pages. They’re lived experiences, backed by medical facts, meant to help you avoid the same traps.
Sick Day Rules for Diabetes: Insulin, Hydration, and Ketone Checks
Nov 22, 2025, Posted by Mike Clayton
Learn the essential sick day rules for diabetes: never skip insulin, check blood sugar every few hours, stay hydrated with the right fluids, and test for ketones to prevent dangerous complications like diabetic ketoacidosis.
MORESEARCH HERE
Categories
TAGS
- treatment
- online pharmacy
- dietary supplement
- side effects
- generic drugs
- medication adherence
- medication safety
- health
- dietary supplements
- health benefits
- online pharmacy Australia
- generic substitution
- adverse drug reactions
- thyroid disorders
- gabapentin
- treatment option
- calcipotriol
- blood pressure
- erectile dysfunction
- closer look
